Scientists have developed potential new therapies that selectively remove aggregated tau proteins associated with Parkinson’s disease. Alzheimerand improve symptoms of neurodegeneration in mice.
Promising therapy against Alzheimer’s
The team of scientists from the Medical Research Council Laboratory of Molecular Biology (MRC LMB) in Cambridge, UK, and the UK Dementia Research Institute (UK DRI) at the University of Cambridge, say that this promising approach could in the future be applied to other brain disorders caused by proteins clumping together inside cells, such as motor neuron disease, Huntington’s disease and Parkinson’s disease.
In two articles, published on Cell and Science demonstrate how harnessing the unique capabilities of a protein called TRIM21 provides potential therapies with two key advantages.
First, they destroy only the tau aggregates linked to Alzheimer’s disease, leaving healthy tau proteins intact. And second, the therapies remove tau aggregates already formed in mice, not just prevent new ones from forming.
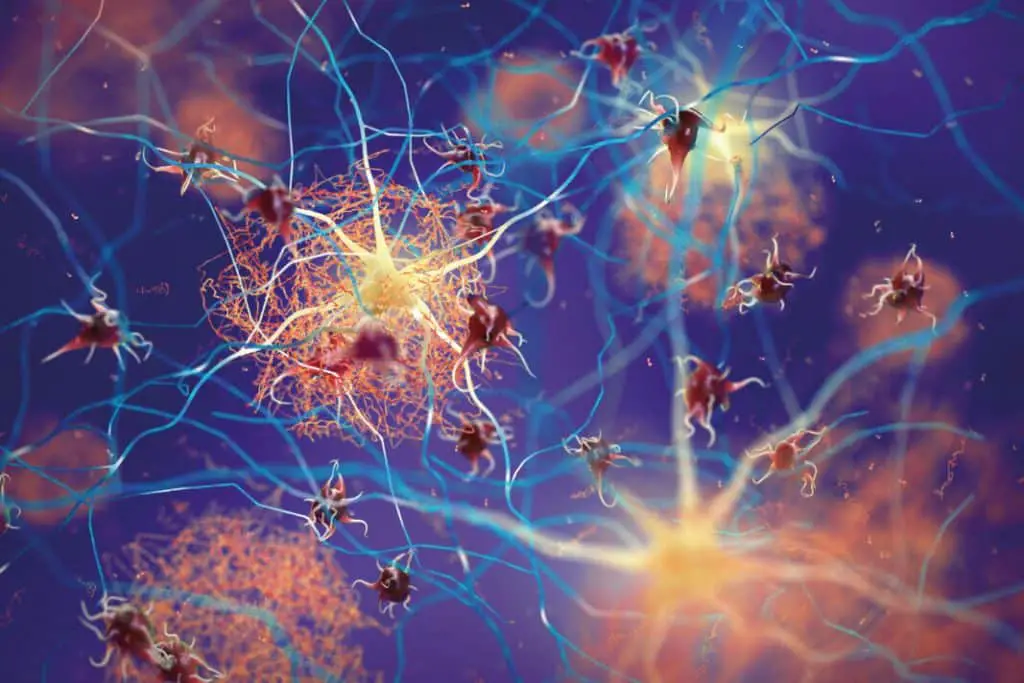
There are two main proteins that fold abnormally and accumulate in aggregates in the brains of people with Alzheimer’s disease: tau and amyloid.
Alzheimer’s amyloid aggregates form in the spaces between brain cells and are being targeted by new antibody therapies, such as lecanemab.
In contrast, tau “tangles” form primarily within nerve cells, although aggregates can spread from cell to cell, which is strongly associated with cognitive decline as the disease progresses.
Antibody therapies have difficulty accessing tau inside cells, so they do not remove existing tau aggregates within cells, but at best prevent their spread.
Other techniques to target tau inside cells, such as antisense oligonucleotides (ASOs), have been shown to reduce tau in promising early clinical trials. However, they target all tau in the brain and therefore remove “healthy” tau as well; the long-term side effects of this are not yet known.
“Healthy” tau protein normally helps provide structural support within nerve cells in the brain, acting as a kind of scaffolding.
This new technique for targeting tau tangles exploits a 2010 discovery by Dr Leo James’s lab at the MRC Laboratory of Molecular Biology into the role of a unique protein called TRIM21, which is a key part of the immune response to viruses.
Outside the cell, the body produces antibodies that bind to invading viruses. When the antibody-bound virus enters a cell, TRIM21 detects it and labels it as “garbage,” delivering it to the cell’s “garbage chute,” the proteasome, for destruction.
The same team, working at the UK’s DRI and MRC LMB, showed in 2023 that TRIM21 could be repurposed to destroy tau protein aggregates associated with Alzheimer’s disease. By replacing virus-binding antibodies with tau-binding antibodies, TRIM21 was repurposed to send tau aggregates to be destroyed via the proteasome.

TRIM21 is particularly well suited for this purpose because of a special feature: a part of the protein called the “RING” that is activated only when two or more TRIM21 proteins cluster together. This means that it is activated and marks its target for destruction only when TRIM21 proteins are bound to adjacent, aggregated tau proteins.
In the new studies, scientists used TRIM21 to create two new therapies that target tau aggregates.
The first therapy, called “RING-nanobody,” combines a tau-binding nanobody, a miniature version of an antibody, with TRIM21 RING.
The second therapy, “RING-Bait,” has the TRIM21 RING attached to a copy of the tau protein itself. The RING-bound tau protein acts as bait: the aggregates incorporate it, and the TRIM21 RING is incorporated as well. Once more RING-Bait is added to the aggregate, it becomes activated and causes the entire aggregate to be destroyed.
The researchers administered DNA encoding TRIM21 therapies to cells containing aggregated tau and found that it cleared away the tau tangles. As hoped, the “healthy” tau remained intact.
Dr Will McEwan, co-lead of the studies, from the UK Dementia Research Institute at the University of Cambridge, said: “Tau aggregates are hidden inside brain cells and very difficult to break down. It is crucial that these new TRIM21-based therapies can be delivered directly into cells, where most tau aggregates reside.
“We’ve found a way that not only degrades tau aggregates, but leaves healthy tau intact to do its job. The new strategy goes beyond what can be achieved with current ASO therapies that are being tested, as it could avoid any potential long-term side effects of clearing normal tau.”

Because different neurodegenerative diseases can have different types of misfolded tau, they tested the therapies on cells containing aggregated tau proteins from brain tissue donated by people with Alzheimer’s disease or progressive supranuclear palsy, which have different misfolded tau structures. The RING-Bait therapy was able to prevent tau aggregation induced by proteins from both the brains of Alzheimer’s and progressive supranuclear palsy patients.
Co-lead study co-author Dr Leo James, from the MRC Laboratory of Molecular Biology in Cambridge, said: “Neurodegenerative diseases can have tau proteins that misfold in many different ways, raising the possibility of needing a different treatment for each disease. One useful aspect of RING-Bait is that, because it is attached to a tau protein, it is a universal Trojan horse that should be incorporated into different types of tau aggregates just like the cell’s own misfolded tau protein.”
For the treatment to work in an animal, it must not only enter the brain, but also the cells within it. To do this, the researchers used a harmless virus that had previously been developed to deliver therapies like this, called adeno-associated virus (AAV). It delivers instructions to DNA to make customized proteins inside brain cells.
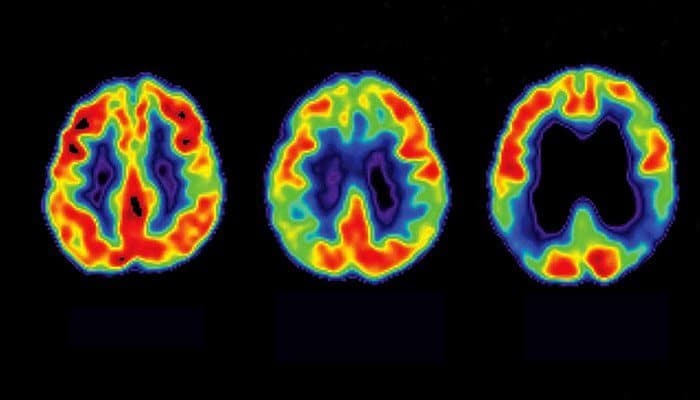
Older mice with tau protein aggregates were injected with a single dose of the gene therapy vector containing the treatment or a placebo.
Within a few weeks, a significant reduction in the amount of aggregated tau was observed in the brain cells of the treated animals.
Importantly, mice treated with RING-Bait slowed the progression of neurodegeneration symptoms and showed significantly improved motor function, as assessed by an artificial intelligence program that evaluated their ability to run.
Study author Dr Lauren Miller, who worked at both the UK Dementia Research Institute and the MRC Laboratory of Molecular Biology, said: “It was not known whether specifically removing tau aggregates within the cell would be sufficient to halt the progression of the disease.
“It is encouraging that a RING-Bait approach reduces disease severity in our model systems, as this suggests that selective removal of tau aggregates is a viable therapeutic approach. Further studies will be needed to demonstrate that this beneficial effect is seen in more human disease models.”
Study author Dr Guido Papa, from the MRC Laboratory of Molecular Biology, said: “The beauty of RING-Bait lies in its broad adaptability and potential to address other conditions characterised by the accumulation of pathological protein clusters.
“Other neurodegenerative diseases are caused by aggregates formed by other proteins, such as TDP43 in motor neuron disease and alpha-synuclein in Parkinson’s disease. It is hoped that RING-Bait will enable the development of future therapies that directly target the aggregation process in these diseases.”
Scientists caution that these Alzheimer’s therapies still need much development before they can be tested in humans, particularly in developing an AAV vector that can safely and effectively deliver RING-nanobody or RING-bait therapies to cells throughout the human brain.
Dr Jonathan Benn, an author of the Alzheimer’s study from the UK Dementia Research Institute at the University of Cambridge, said: “It is important to stress that although we have shown that it works in a mouse model, we are a long way from a therapy that could be used in humans. It would be important to establish whether it is safe to use TRIM21-based therapies in the human brain and whether the treatments are effective in both clearing the aggregates and improving the course of the disease.
“Some AAV vectors are already approved for use in humans, for example in degenerative eye diseases and genetic diseases such as spinal muscular atrophy. However, getting enough AAV into the adult brain remains a significant challenge: the human brain is about 1,000 times larger than a mouse brain. But this is a rapidly evolving field and there are cutting-edge gene delivery methods that we hope will allow our therapies to be delivered at scale in the future.”
#Alzheimers #Therapy #Targets #Destroys #Tau #Tangles
