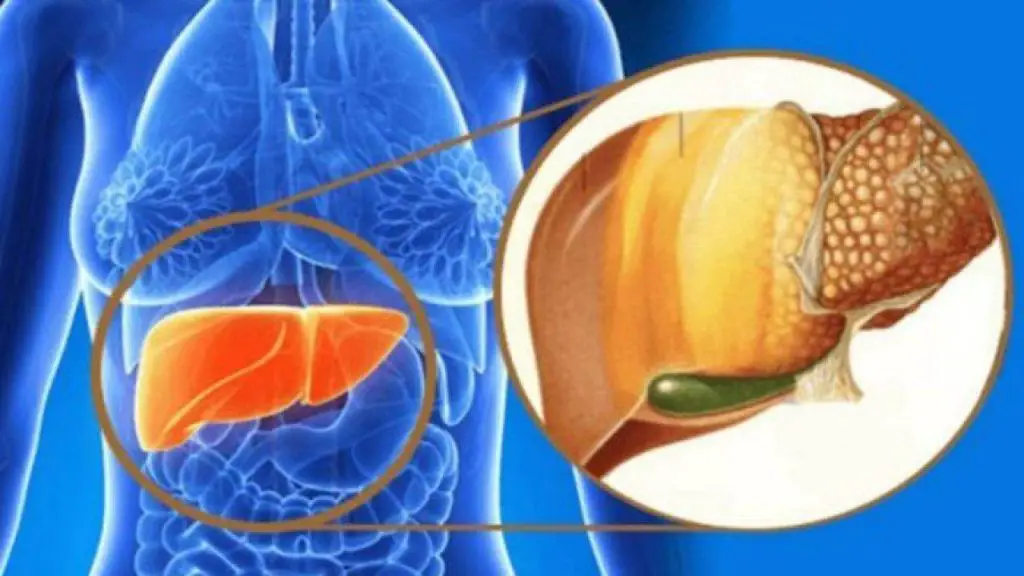
Researchers at Edith Cowan University (ECU) are studying the effects that ellagic acid, an antioxidant found in some fruits and vegetables, could have in halting and potentially reversing the damage caused by the disease liver fat.
The study was published in the journal Antioxidants.
Can pomegranates combat fatty liver disease?
Non-alcoholic fatty liver disease (NAFLD) is the physiological manifestation of obesity in the liver. The prevalence of fatty liver disease has increased from 25.24% in 2015 to 29.38% in 2021, and this condition now accounts for 45.8% of all cases of chronic liver disease-related deaths worldwide.
There is currently no treatment for the long-term management of NAFLD; however, dietary interventions have been studied to treat this disease, including several polyphenolic compounds such as ellagic acid.
ECU researcher Dr. Lois Balmer and Ph.D. student Tharani Senavirathna noted that ellagic acid, found in a variety of foods such as raspberries, pomegranate, blackberries, and pecans, is widely recognized for its antioxidant properties , but also has anti-inflammatory, antifibrotic and anti-tumor properties.

“Ellagic acid stands out as a remarkable polyphenolic compound, possessing a wide range of pharmacological properties that hold promise in the treatment of various chronic diseases, including fatty liver disease.
“Due to its multiple biological effects, edible plants containing ellagic acid and its derivatives are recognized as valuable functional foods for improving human health. Furthermore, there is evidence to suggest that ellagic acid, when combined with other antioxidant nutraceuticals, displays a synergistic therapeutic effect, making it a potential candidate for combination therapy.”
Ms Senavirathna was involved in a previously undertaken pilot study investigating the effects of several polyphenolic compounds on fatty liver disease, with ellagic acid proving the most promising in reducing inflammation.
A larger study is currently underway which will also examine at what point in the disease treatment would be ineffective in reversing liver damage.
Amino acid linked to NAFLD could provide clues to treatment
One study also implicates low levels of the amino acid glycine in the development of non-alcoholic fatty liver disease or fatty liver disease. It also suggests that addressing this issue could be key to future treatment of the disease.
“We have discovered a new metabolic pathway and a potential new treatment,” says senior author Y. Eugene Chen, M.D., Ph.D., professor of internal medicine and surgery, of the Michigan Medicine Frankel Cardiovascular Center. His team collaborated with researchers from the University of Michigan, Wayne State University and the Technion-Israel Institute of Technology.
Chen says there is a great need to expand treatment options for NAFLD patients. Although it is the most common chronic liver disease, there are currently no drugs approved to treat it.

Lead author Oren Rom, Ph.D., RD, a researcher at the Michigan Medicine Frankel Cardiovascular Center, says the team focused on the poorly understood relationship between dysregulated amino acid metabolism and fatty liver disease.
“Notably, low circulating glycine is consistently reported in patients with NAFLD and related comorbidities including diabetes, obesity, and cardiovascular disease,” says Rom. “Our studies not only offer a metabolic explanation for defective glycine metabolism in NAFLD, but also discover a potential glycine-based treatment.”
Researchers were able to improve body composition and many other measurements in mouse models using a tripeptide known as DT-109.
“Glycine treatment attenuates experimental fatty liver disease by stimulating hepatic fatty acid oxidation and glutathione synthesis, thus warranting clinical evaluation,” the authors write.
Connection between fatty liver disease and rare pregnancy complications
A new link has been found between a rare and serious condition that typically presents as itchy hands during pregnancy and the world’s most common chronic liver disease, according to research presented at Digestive Disease Week (DDW). Researchers have found that intrahepatic cholestasis of pregnancy (ICP), a bile acid disorder in adults that affects approximately one in 300 pregnancies, may be associated with nonalcoholic fatty liver disease (NAFLD).
“Intrahepatic cholestasis of pregnancy is characterized by the accumulation of bile acids during pregnancy and is associated with an increased risk of fetal death if left untreated,” said co-author Erica Monrose, MD, of the Icahn School of Medicine at Mount Sinai , New York, New York. “Fatty liver disease, on the other hand, has been linked to dysregulation of bile acids, but their role is not well understood. Our research shows that there is a connection between altered bile acid metabolism in both disease processes, which may have implications for the future. management of NAFLD.”
The study examined medical records from 149 pregnancies complicated by ICP among a largely Latino population, one of three ethnic groups, along with Bangladeshi and Swedish women, most often found to have ICP.
The researchers compared the ICP pregnancies to a control group of 200 women, through liver imaging and other criteria. They found that women with ICP were 5.7 times more likely to have a diagnosis of fatty liver disease than patients in the control group.

“In the search for therapeutic drugs for fatty liver disease, scientists need a better understanding of the role bile acids play in disease progression,” said Dr. Monrose. “If the connection is confirmed, ICP could prove to be a new model through which to study bile acid metabolism in patients with NAFLD.”
In the United States alone, fatty liver disease, which is often treated with dietary changes, affects an estimated 80 to 100 million people and has become the second leading cause of liver transplantation and the leading cause among women.
“In addition to helping solve the mystery of NAFLD, our study also suggests that patients with ICP should be seen by a liver specialist because they may develop chronic liver disease,” said Dr. Monrose.
Given these findings, further research should examine differences in NAFLD progression in women who had fatty liver disease and subsequently were diagnosed with ICP, compared to women with NAFLD who did not develop ICP. Furthermore, since bile acids have been implicated in the progression of NAFLD, future research should investigate possible differences in NAFLD progression between ICP patients and their counterparts.
Finally, patients with NAFLD who develop ICP may benefit more from drugs developed that target bile acid metabolism pathways.
HIV-infected individuals at high risk for fatty liver disease and progressive liver disease
The increasing burden and risk of non-alcoholic fatty liver disease (NAFLD) associated with HIV infection were highlighted today in two studies presented at the 2019 International Liver Congress in Vienna, Austria.
These studies found that while prevalence and mortality rates associated with viral hepatitis in HIV-infected individuals are declining, rates associated with fatty liver disease are increasing, leading to a risk of progressive liver disease.
People living with HIV infection appear to be at greater risk of developing NAFLD than the general population. The prevalence of NAFLD worldwide has been estimated at 25%, while the prevalence in HIV populations has been much higher in most reported studies.
Fatty liver disease represents a major risk factor for the development and progression of liver disease,5 and with the availability of antiviral drugs effective against hepatitis B and C, it is conceivable that NAFLD may become the liver disease in the future most important affecting individuals with HIV.
The first study presented in Vienna aimed to evaluate the prevalence and mortality trends of NAFLD, viral hepatitis and other liver diseases in HIV-infected subjects.
We examined data from >47,000 HIV-infected Medicare recipients in the United States and identified >10,000 individuals with liver disease: 5,628 with HCV-related disease, 1,374 with HBV-related disease, 645 with HBV-related disease HCV/HBV, 2,629 with fatty liver disease and 198 with other liver diseases.
During the 10 years between 2006 and 2016, viral hepatitis prevalence rates decreased from 27.75 to 24.17 per 100,000 population (p=0.009), while NAFLD rates more than doubled from 5, 32 to 11.62 per 100,000 inhabitants (p<0.001).
Viral hepatitis-related mortality rates also decreased from 3.78 to 2.58 per 100,000 population (p=0.006), while NAFLD-related mortality increased from 0.18 to 0.80 per 100,000 population (p =0.041).
“Our study demonstrates that as highly effective treatments for HBV and HCV infections lead to reduced associated mortality in HIV-infected populations, fatty liver disease is becoming an increasingly important cause of liver disease,” he said Dr. Zobair Younossi, professor and chair of the Department of Medicine at the Inova Fairfax Medical Campus in Falls Church, Virginia, USA, who presented the study results.
The second study, involving teams from Canada, the United Kingdom and Italy, used a diagnostic algorithm based on current EASL guidelines in HIV-negative populations6 to identify individuals with NAFLD from two cohorts of HIV-infected adults without a significant alcohol consumption or viral hepatitis coinfection. (the LIVEr disease in HIV [LIVEHIV] and the cohorts of the Modena HIV Metabolic Clinic [MHMC]). Of 1,228 HIV-infected individuals screened (mean age, 50 years; 73% male; time since diagnosis, 16 years), 31.8% had NAFLD.
Based on elevated alanine aminotransferase (ALT) levels and/or significant fibrosis, 25.2% of these patients were considered at risk for progressive liver disease compared to 18.4% of patients without fatty liver disease.
Independent predictors of liver disease progression requiring specialist intervention were male sex, diabetes, and duration of HIV infection.
“By applying current NAFLD guidelines developed for HIV-negative populations, we have identified significant proportions of HIV-infected patients at risk of fatty liver disease and progressive liver disease,” said Dr Sila Cocciolillo of the Royal Victoria Hospital , McGill University Health Centre, Montreal, Canada.
“We believe this supports the need for dedicated monitoring of these patients, with referral to hepatology services when necessary.”
Professor Philip Newsome (Deputy Secretary, EASL) said: “These studies point to the changing profile of liver disease in patients with HIV: while viral hepatitis is still the main cause of liver disease in such groups, HIV disease Fatty liver is becoming a much more common problem. This reinforces the need to study therapeutic agents in patients with NAFLD and HIV, an area that is rarely examined.”
#Fatty #liver #disease #solution #pomegranates