In the rapidly evolving field of neuroscience, the brain stimulation noninvasive represents new hope for understanding and treating myriad neurological and psychiatric conditions without surgery or implants.
The researchers, led by Friedhelm Hummel, holder of the Defitchech Chair in Clinical Neuroengineering at EPFL’s School of Life Sciences, and postdoc Pierre Vassiliadis, are pioneering a new approach in the field, opening frontiers in the treatment of conditions such as addiction and the Depression.
The study was published on Nature Human Behavior
Deep brain stimulation: the new frontier for the treatment of mental suffering
Neurological disorders, such as addiction, depression and obsessive-compulsive disorder (OCD), affect millions of people around the world and are often characterized by complex pathologies involving multiple brain regions and circuits. These conditions are notoriously difficult to treat due to the complex and poorly understood nature of brain function and the difficulty of delivering therapies to deep brain structures without invasive procedures.
The research, exploiting Transcranial Temporal Electrical Brain Stimulation (tTIS), specifically targets the deep regions of the brain which are the control centers of several important cognitive functions and involved in various neurological and psychiatric pathologies.
The study highlights the interdisciplinary approach that integrates medicine, neuroscience, computer science and engineering to improve our understanding of the brain and develop potentially life-changing therapies.
“Invasive deep brain stimulation (DBS) has already been successfully applied to deeply located neural control centers to curb addiction and treat Parkinson’s, OCD or depression,” says Hummel. “The key difference with our approach is that it is non-invasive, meaning we use low-level electrical stimulation on the scalp to target these regions.”

Vassiliadis, lead author of the paper, a doctor with a joint PhD, describes tTIS as using two pairs of electrodes attached to the scalp to apply weak electric fields inside the brain.
“Until now, we could not specifically target these regions with non-invasive techniques, as low-level electric fields would stimulate all regions between the skull and deeper areas, making any treatment ineffective. Brain stimulation allows us to selectively stimulate deep regions of the brain that are important in neuropsychiatric disorders,” she explains.
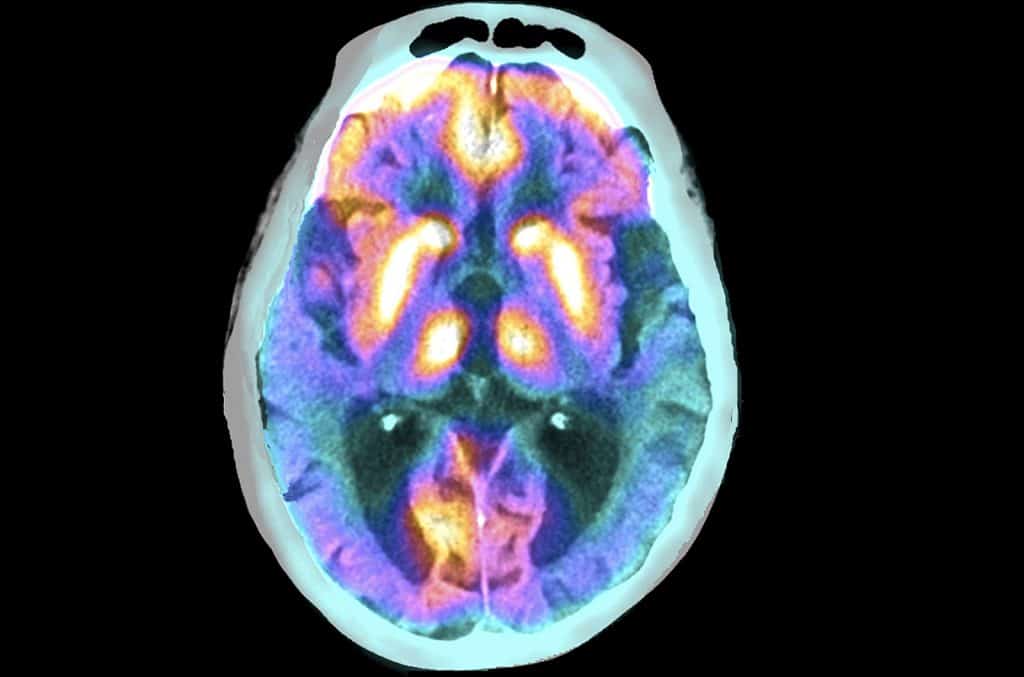
The innovative technique is based on the concept of temporal interference, initially explored in rodent models and now successfully translated into human applications by the EPFL team. In this experiment, one pair of electrodes is set to a frequency of 2,000 Hz, while the other is set to 2,080 Hz.
Thanks to detailed computational models of the brain structure, the electrodes are placed specifically on the scalp to ensure that their signals intersect in the target region.
This is where the magic of interference happens: the slight frequency disparity of 80 Hz between the two currents becomes the actual stimulation frequency within the target zone. The brilliance of this method lies in its selectivity; high base frequencies (e.g., 2,000 Hz) do not directly stimulate neural activity, leaving intermediate brain tissue unaffected and concentrating the effect exclusively on the target region.
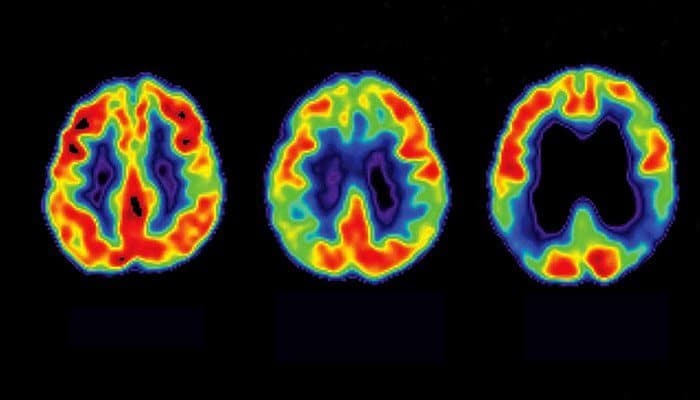
The focus of this latest research is the human striatum, a key player in reward and reinforcement mechanisms. “We’re looking at how reinforcement learning, essentially how we learn through rewards, can be affected by targeting specific brain frequencies,” Vassiliadis says. By applying brain stimulation to the striatum at 80 Hz, the team found that they could disrupt its normal functioning, directly affecting the learning process.
The therapeutic potential of brain stimulation is immense, particularly for conditions such as addiction, apathy and depression, where reward mechanisms play a crucial role.
“Also, for example, people tend to get too close to rewards. Brain stimulation could help reduce this pathological over-emphasis,” emphasizes Vassiliadis, who is also a researcher at the Institute of Neuroscience at UCLouvain.

Furthermore, the team is exploring how different patterns of brain stimulation can not only disrupt but also potentially improve brain function. “The first step was to demonstrate the hypothesis that 80 Hz affects the striatum, and we did this by interrupting its functioning.
Our research also shows promise in improving motor behavior and increasing striatum activity, particularly in older adults with reduced learning abilities,” Vassiliadis adds.
Hummel, a trained neurologist, sees brain stimulation as the beginning of a new chapter in brain stimulation, offering personalized treatment with less invasive methods. “We are looking at a non-invasive approach that allows us to test and personalize the deep brain stimulation treatment in the early stages,” he says.
Another key benefit of brain stimulation is its minimal side effects. Most participants in their studies reported only mild sensations on the skin, making it a highly tolerable and patient-friendly approach.
Hummel and Vassiliadis are optimistic about the impact of their research. They envision a future where noninvasive neuromodulation therapies could be readily available in hospitals, offering a cost-effective and expansive treatment scope.
Brain stimulation without surgery could provide a new treatment for dementia
Scientists at Imperial College London are leading the development and testing of a new method of brain stimulation, which could provide an alternative treatment for brain diseases such as Alzheimer’s and associated memory loss.
Known as temporal interference (TI), the non-invasive method of brain stimulation works by delivering electrical fields to the brain through electrodes placed on the patient’s scalp and head.
By targeting the overlapping electric fields the researchers were able to stimulate an area deep in the brain called the hippocampus, without affecting surrounding areas, a procedure that until now required surgery to implant electrodes in the brain.
Brain stimulation has been successfully trialled for the first time with 20 healthy volunteers by a team from the UK Dementia Research Institute (UK DRI) at Imperial and the University of Surrey.
Their initial findings, published in the journal Nature Neuroscience, show that when healthy adults perform a memory task while receiving TI stimulation, this helps improve memory function.
The team is now conducting a clinical trial on people with early-stage Alzheimer’s disease, in the hope that TI could be used to improve symptoms of memory loss.
Dr Nir Grossman, from the Department of Brain Sciences at Imperial College London, who led the work, said: “Until now, if we wanted to electrically stimulate structures deep within the brain, we had to surgically implant electrodes which obviously pose risks to the patient and can lead to complications.
“With our new technique we have demonstrated for the first time that remote brain stimulation of specific deep regions of the human brain is possible without the need for surgery. This opens up a completely new avenue of treatment for brain diseases such as Alzheimer’s that affect deep brain structures.”
TI was first described by the Imperial College London team in 2017 and shown to work in principle in mice.
This latest work shows for the first time that brain stimulation is effective in stimulating deep regions of the human brain. According to the researchers, this could have broad applications and will allow scientists to stimulate different deep regions of the brain to discover more about their functional roles, accelerating the discovery of new therapeutic targets.
In the study, the researchers first used post-mortem brain measurements to verify that electric fields could be remotely focused on the hippocampus, a curved structure deep in the brain that plays a critical role in memory and learning.
The team then applied brain stimulation to healthy volunteers as they memorized pairs of faces and names, a process highly dependent on the hippocampus. Using functional magnetic resonance imaging (fMRI), researchers demonstrated that TI selectively influences hippocampal activity evoked by the memory task.
Finally, the researchers repeated the brain stimulation for a longer period of 30 minutes. This demonstrated that TI stimulation during the task leads to improved memory accuracy.
Dr Ines Violante, from the University of Surrey and Honorary Research Fellow at Imperial, and first author of the study, said: “The ability to selectively target deep areas of the brain using a non-invasive approach is very exciting as it provides a tool to investigate how the human brain works and opens possibilities for clinical applications.”
“The combination of non-invasive imaging and brain stimulation will help us unravel the processes that support our cognitive functions, such as memory and learning. Knowledge of these processes and how they can be altered is essential to develop better individualized strategies to treat or delay the onset of disease.”
Dr Grossman added: “We hope this work will help increase the availability of deep brain stimulation therapies while dramatically reducing costs and risks.”
“We are now testing whether repeated treatment with stimulation over a number of days could benefit people in the early stages of Alzheimer’s. We hope this will restore normal brain activity in the affected areas, which may improve symptoms of memory impairment.”
This study is published at the same time as a second paper led by researchers at the École polytechnique fédérale de Lausanne (EPFL) in Switzerland, who independently validated the technology.
In the EPFL study, also published in Nature Neuroscience, researchers used TI technology to focally stimulate a different deep area of the brain called the striatum and improve motor memory function in healthy volunteers.
#Noninvasive #deep #brain #stimulation #potential #therapy #addiction #depression #obsessive #compulsive #disorder