A new gene therapy treatment for muscular dystrophy of Duchenne shows promise not only in halting the decline of muscles in patients with the inherited genetic disease, but perhaps, in the future, in repairing those muscles. The UW Medicine-led research focuses on delivering a series of protein packages into shuttle vectors to replace the defective DMD gene in muscles. The added genetic code will then begin to produce dystrophin, the protein missing in patients with muscular dystrophy.
A promising cure for muscular dystrophy
There is currently no cure for the disease and available treatments and drugs only slow the disease. In the case of Duchenne muscular dystrophy, the subject of this study, patients, all male because the gene is on the X chromosome, begin to show symptoms around age 4 and usually die in their 20s or 30s.
The results of the new gene therapy were published today in Nature.
UW Medicine neurologist and geneticist Dr. Jeffery Chamberlain, the study’s lead author, has spent his career researching therapies and finding a cure for muscular dystrophy. He is the director of the Wellstone Muscular Dystrophy Research Center and the McCaw Chair in Muscular Dystrophy at the University of Washington School of Medicine. The research project was led by molecular biologist Dr. Hichem Tasfaout, who works in Chamberlain’s lab.
What has stymied researchers in the past is that the gene being repaired is the largest gene in nature, Chamberlain noted. Until now, there has been no way to deliver adequate protein fixes into muscles.
“Imagine having a king-size bed delivered to your home that doesn’t fit through the door,” he said.
The new method, which has been successful in mouse models, uses a series of adeno-associated viral vectors, or AAVs, which are small shuttles derived from a virus that are used to deliver gene therapies into human cells. Instead of an AAV, this gene therapy uses a series of AAVs that take parts of the therapeutic protein into the muscles, along with embedded instructions to begin assembling the necessary genetic fix once inside the body.

Returning to the king-size bed analogy, not only are the parts picked up piece by piece, but delivery men begin assembling the bed once it’s inside the home. The next step for the therapy is human trials, which are expected to begin in about two years, Chamberlain said.
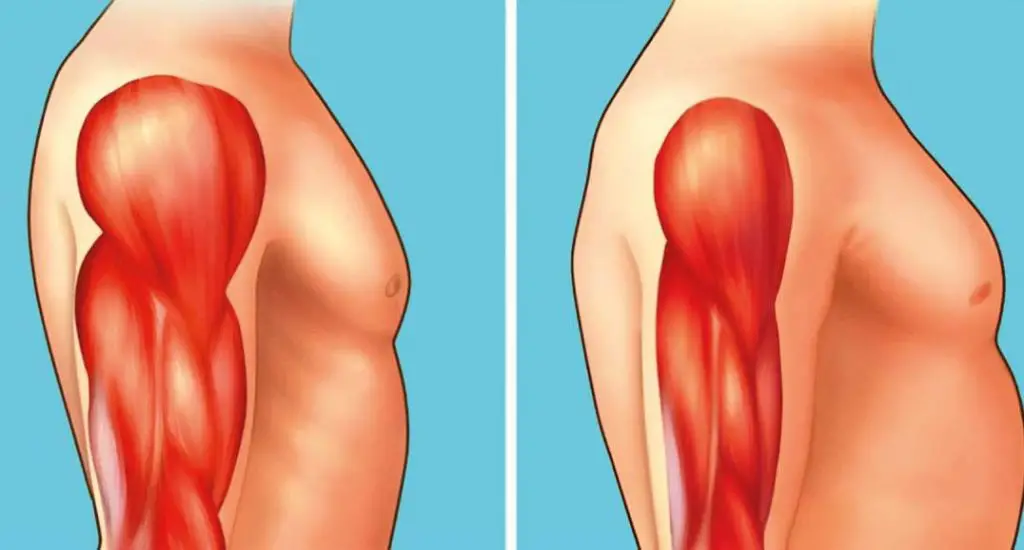
In the lab, this method not only stopped further progression of the disease, but was able to reverse much of the pathology associated with the dystrophy. Eventually, Chamberlain and Tasfaout hope that this method could lead to a reversal of muscle atrophy and restore normal muscle tissue health.
The newer approach also uses a new type of AAV vector that allows for the use of lower doses and therefore may reduce or eliminate some of the side effects of earlier approaches, Chamberlain said.
“When we infuse a high dose of these delivery shuttles, the body goes, ‘Wow, what’s going on here?’” he said.
This triggers an immune response that can damage the heart or liver, he explained.
This triggers an immune response that can damage the heart or liver, he explained.
Chamberlain remembers watching the Jerry Lewis Telethon as a kid and wanting to help those kids. That feeling may have been the spark for the passion that ultimately drove his career. He ended up being an expert who discussed the science of therapies on the telethon about seven times.
“Meeting the families and patients motivated me to try even harder,” she said.
Zebrafish eye muscles give hope to people with muscular dystrophy
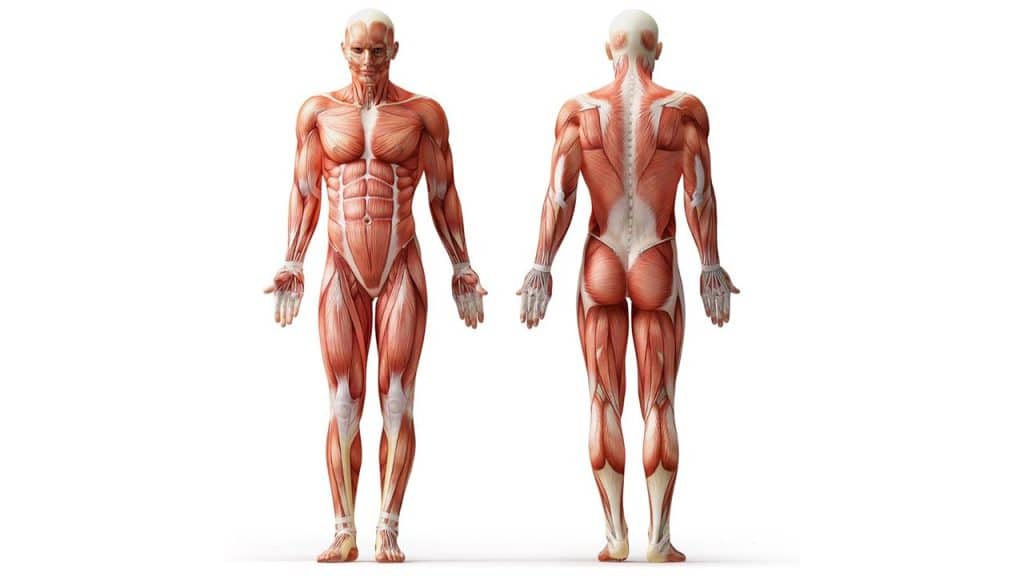
Muscular dystrophies are a group of diseases in which proteins in muscles do not function properly, either through inherited or spontaneous mutations. This, in turn, leads to the breakdown of muscle tissue over time and patients eventually become wheelchair-bound and often die prematurely because the muscles that help with breathing or the heart stop working.
The muscles that control eye movements function well throughout the disease, making it important to study them to try to discover what strategies they use to survive muscular dystrophies.
“In my research I studied the eye muscles of zebrafish, which have been shown to have the same properties in human muscular dystrophies, and then generated new disease models with the help of the Crispr/Cas9 genetic scissors,” says Nils Dennhag.
“By reading gene expression in the eye muscles of zebrafish, both healthy and affected by muscular dystrophies, we were able to partially decipher how the eye muscles manage these diseases, through the positive regulation of the protein Fhl2.”
Fhl2 protects muscle fibers in the eye muscles by preventing cell breakdown and slowing unnatural pathological enlargement. Fhl2 is not found naturally in large areas of muscle in zebrafish or humans, but by genetically forcing Fhl2 gene expression here, researchers were able to demonstrate a large increase in survival in zebrafish with the most lethal type of muscular dystrophy: Duchenne muscular dystrophy.
In addition to improved survival, zebrafish with Duchenne muscular dystrophy that also had increased Fhl2 expression had healthier muscle fibers, significantly better innervation, and better swimming ability than diseased zebrafish without Fhl2. Additionally, broken fibers regenerated faster, leading to better recovery.
“Overall, our studies show that it is possible to use eye muscles as a kind of model for how to deal with living with muscular dystrophies, which has not been shown before to this extent. We also believe that this may be a way forward for treating humans, as we have also seen that human eye muscles have muscle fibers that express Fhl2.
“We think we’ve only scratched the surface of the strategies that eye muscles can offer, but it’s a good step forward and shows that this new type of treatment approach is possible,” Dennhag says.
“We used CRISPR/Cas9 genetic scissors to create different models of muscular dystrophies, which are used in the study to study how the eye muscles react when these proteins are removed. We then sequenced RNA from both the eye muscles and the body muscles to see what differences existed between these tissues in disease conditions.
When we found that Fhl2 was upregulated in eye muscles, we used circular DNA with the Fhl2 gene, which is linked to a muscle-specific promoter, and injected it into zebrafish with muscular dystrophy. This causes all the muscles in the body to express Fhl2, not just the eye muscles, which led to the effects described above,” Dennhag says.
Some exercises can help those suffering from muscular dystrophy
Muscular dystrophy is a debilitating disease that causes weakness and breakdown of skeletal muscles, which progressively worsens over time. According to a team of researchers from the University of Maine, certain activities can help strengthen the muscles affected by muscular dystrophy, and they discovered this by stimulating zebrafish and observing them as they exercised.
Zebrafish are an effective test model for muscular dystrophy, due to the molecular similarities between zebrafish muscles and human muscles. Zebrafish can also be bred with a mutation that closely models Duchenne muscular dystrophy, a severe type of muscular dystrophy that affects boys.
However, zebrafish can’t lift weights, so the UMaine researchers used a process called neuromuscular electrical stimulation (NMES), which stimulates specific nerves to cause muscles to contract. The researchers designed four NMES regimens and named them after four common weight-lifting routines: power, strength, hypertrophy, and endurance. The zebrafish were then placed in a 3D-printed underwater “gym” made of tunnels and electrodes, and the researchers scanned their skeletal muscles to see how they had changed.

The study found that while each of the NMES weight-lifting “routines” differently affected neuromuscular junction morphology, swimming, and survival in zebrafish, only one, resistance neuromuscular stimulation (eNMES), improved all three, provided it was accompanied by a certain antioxidant, heme oxygenase, and a receptor called integrin alpha7.
“eNMES is defined by high-frequency, low-voltage pulses, which is similar to a high-rep, low-weight workout that we would do in a gym. The long-standing consensus in the muscular dystrophy field is that minimizing resistance training preserves strength and muscle mass because it reduces the risk of muscle damage.
“Our data suggest that some level of NMES-induced activity is actually beneficial for overall muscle health,” says Elisabeth Kilroy, first author of the study who conducted the research for her Ph.D. at UMaine. Kilroy is now the director of neuroMuscular ObserVational Research (MOVR) at the Muscular Dystrophy Association.
Research suggests that the right type of resistance training could be beneficial for human patients with muscular dystrophy. There is also potential for NMES to improve mobility and strength in patients with muscular dystrophy, although not much is known about how the technology can be applied in this way.
“I think the most exciting thing is that we have established a model for neuromuscular plasticity in healthy versus diseased muscles, and this model will allow us to elucidate mechanisms that could form the basis for potential future therapies,” says Clarissa Henry, professor of biological sciences, director of the Graduate School of Biomedical Science and Engineering, and principal director of the Henry Lab.
#Muscular #Dystrophy #Gene #Therapy #Offers #Hope
