According to a study published in the Journal of Clinical InvestigationNorthwestern Medicine scientists have uncovered the molecular mechanisms underlying lymphatic valve development, a finding that could prove useful in treating lymphedema.
Molecular mechanisms underlying lymphedema discovered
Lymphedema, a chronic condition that causes localized swelling, has no cure and affects about 1 in 100,000 people in the United States, according to the National Institutes of Health.
In the study, researchers sought to understand how genetic mutations previously associated with lymphedema contribute to the disease, said Dr. Susan Quaggin, chair, Irving S. Cutter Professor of Medicine, and the study’s lead author.
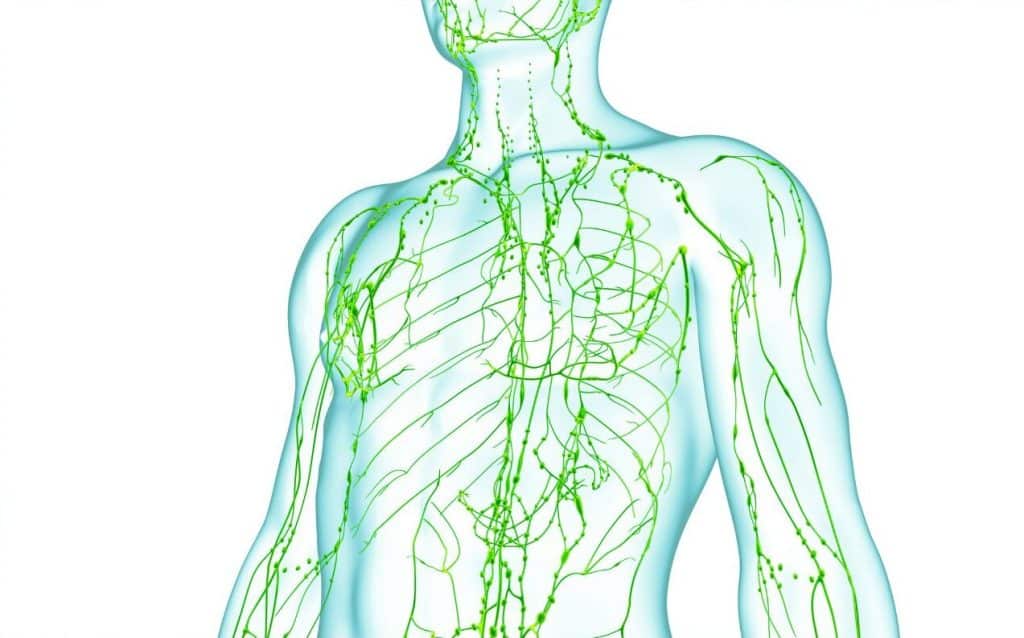
“Lymphedema is a common and debilitating medical condition,” Quaggin said. “The study was designed to unravel the molecules and pathways responsible for the proper development of a functional lymphatic system: disruption of lymphatic development causes lymphedema.”
Previous research has identified mutations in the PIEZO1, ANGPT2, and TIE1 genes as potential culprits in lymphedema.
In the current study, the researchers studied mice lacking these genes to better understand how a healthy lymphatic system develops and how genetic variations can lead to lymphedema.
In the current study, the researchers studied mice lacking these genes to better understand how a healthy lymphatic system develops and how genetic variations can lead to lymphedema.
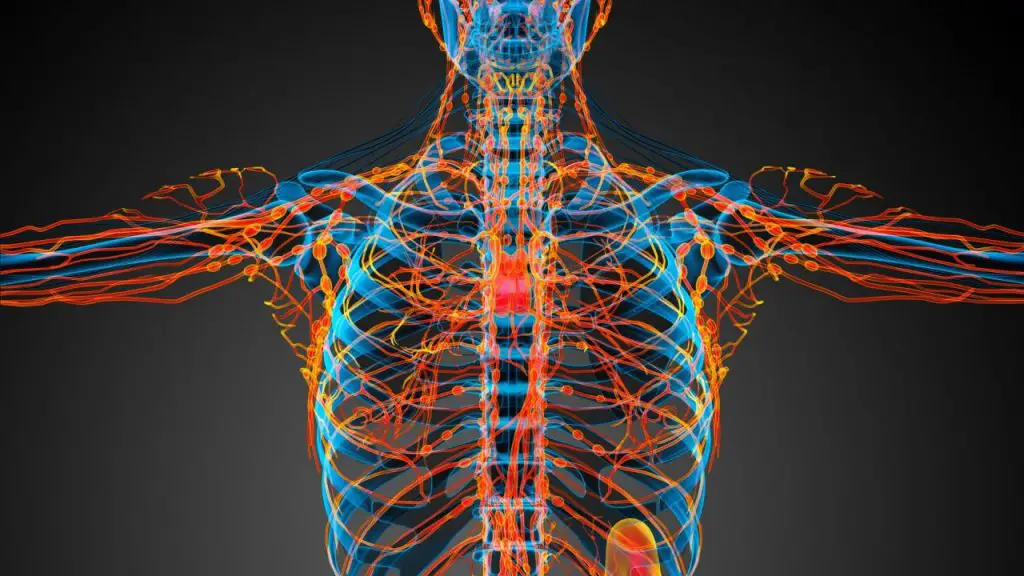
By performing RNA sequencing in mice coupled with cell-based studies, the researchers observed that PIEZO1 activation in lymphatic endothelial cells resulted in rapid exocytosis, the process of vesicles fusing with the plasma membrane and releasing their contents, including the lymphatic growth factor ligand, Angiopoietin-2, outside the cell.
The researchers also observed that this activation increased signaling in genes associated with lymphedema and induced the cells to export FOXO1, a protein known to repress the formation of lymphatic valves.
Overall, the findings provide insight into the genetic regulation of lymphatic function and the molecular pathways involved in lymphedema, Quaggin said.
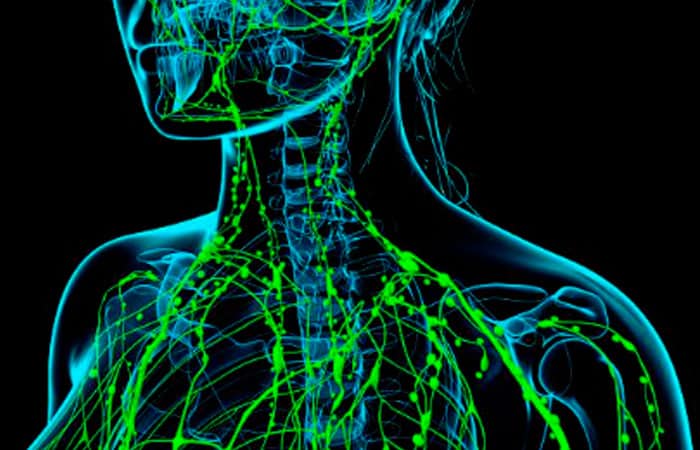
“We identified a new molecular pathway that highlighted how mechanical or physical signals can trigger the development of lymphatic valves in the right place at the right time, precisely at the point where there is likely to be a signal that physical forces require the formation of a valve,” said Quaggin, who also directs the Feinberg Cardiovascular and Renal Research Institute.
Quaggin and his lab will now focus their attention on studying this pathway in blood vessel development, he said.
“We are now studying whether this pathway also holds true in the development of blood and hybrid vessels, particularly in the development of a unique vessel in the anterior part of the eye known as Schlemm’s canal, which is a lymphatic-like vessel,” said Quaggin, who is also a member of the Robert H. Lurie Comprehensive Cancer Center at Northwestern University.
“The reason why it is important to explore Schlemm’s canal is due to the fundamental role this vessel plays in controlling pressure in the eye and preventing the development of glaucoma.”
A new gene involved in primary lymphedema
The Laboratory of Human Molecular Genetics at the de Duve Institute (UCLouvain), headed by Professor Miikka Vikkula, has recently identified mutations in a new gene, ANGPT2, responsible for primary lymphedema. Together with the Wihuri Research Institute and its director, Professor Kari Alitalo at the University of Helsinki, the laboratories were able to demonstrate how these mutations cause the disease.
“The mutations result in the loss of normal function of the protein ANGPT2, which is known to play a role in the maturation of lymphatic and blood vessels. This important discovery opens up possibilities for the development of improved treatments for lymphedema,” explains Professor Alitalo.
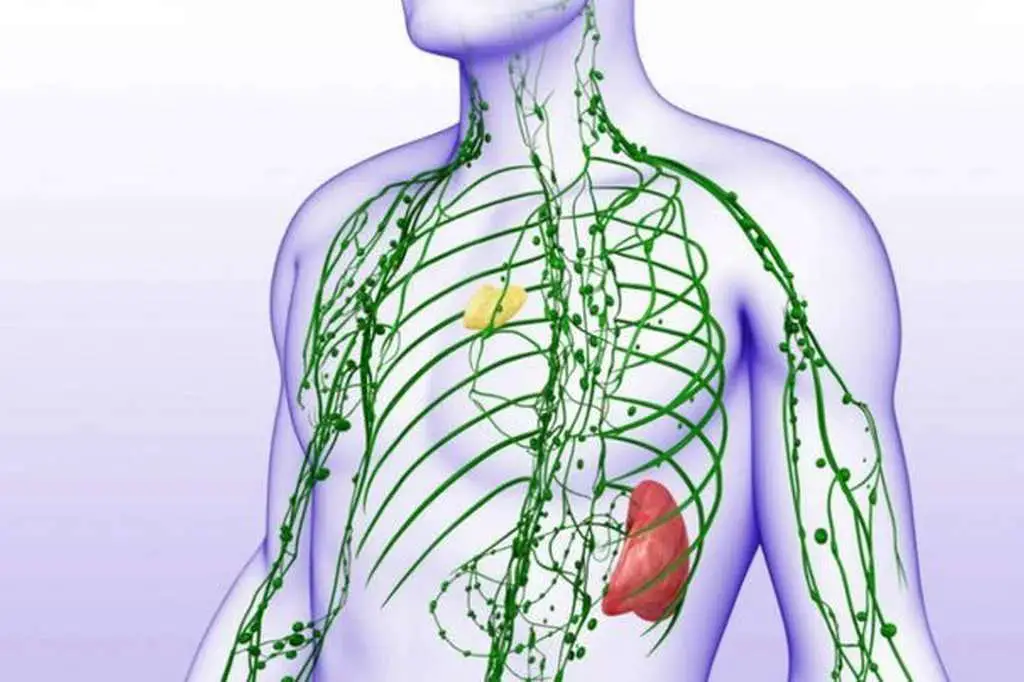
Lymphedema is a chronic, severely disabling disease that results from abnormal development or function of the lymphatic system. In patients, lymph is poorly drained from the tissues and therefore accumulates in the extremities, causing swelling and fibrosis, limiting the mobility of the affected body part and increasing the likelihood of infection. Lymphedema can be primary, which has no known underlying cause, or secondary, when it results from removed or damaged lymph vessels, such as after surgery, infection or cancer treatment. Primary lymphedema is often hereditary.
The team at the de Duve Institute with its large international network of collaborators, including the Center for Vascular Anomalies and the Center for Medical Genetics at the Saint-Luc Hospital in Brussels, collected samples from nearly 900 patients with primary lymphedema, as well as collecting samples from their family members. Using whole-exome sequencing (sequencing all the coding parts of genes in the genome), they discovered mutations in ANGPT2 in lymphedema patients from five families.
ANGPT2 encodes the protein angiopoietin 2, a growth factor that binds to receptors in blood and lymph vessels, first identified in Professor Alitalo’s laboratory.
“ANGPT2 has been shown previously to influence lymphatic development in mice, but this is the first time that mutations in this gene have been found to cause lymphedema in humans,” says Professor Alitalo.
Of the mutations identified, one deletes a copy of the entire gene, while the other four are amino acid substitutions. The researchers showed that three of the mutants are not secreted properly by cells that normally produce the protein, and this also decreases the secretion of the protein produced by the remaining normal allele. Thus, the mutations had a so-called dominant-negative effect. The fourth mutant was hyperactive in inducing increased proliferation of dilated lymphatic vessels. This mutant demonstrated impaired integrin binding.
The mutations that caused primary lymphedema in patients provided important insights into the function of the ANGPT2 protein and the mechanisms that lead to lymphedema.
In Europe, more than 1 million people have lymphedema. Treatment is limited to repeated manual lymphatic massage and the use of compression garments to reduce tissue swelling. Surgery may be helpful in some cases. Another lymphatic vessel growth factor, VEGF-C, is currently undergoing clinical trials in combination with surgery to treat lymphedema in patients whose lymph nodes in the armpit have been removed due to metastatic breast cancer. There is currently no cure for lymphedema, and it resolves or improves over time in only a minority of cases.
“Identifying the genetic causes is essential for better management of the disease. It allows for a more precise and reliable diagnosis, whereas today many people with the disease are still undiagnosed. As the study just published shows, research on lymphedema leads to understanding the underlying cellular mechanisms, which could be targets for the development of new therapies,” says Professor Alitalo.
Another way to detect lymphedema
Bioimpedance spectroscopy (BIS) is a noninvasive technology that measures the amount of fluid in a limb. It works by sending a low-level electrical current through the arm or leg and measuring the resistance to the current (impedance).
In this way, the BIS can detect lymphedema, a swelling caused by a blockage of the lymphatic system that occurs in a fifth of patients after breast cancer treatment.

Breast cancer treatment-related lymphedema (BCRL) has been effectively detected using the BIS dual-tab electrode. Paula Donahue, DPT, MBA, and colleagues tested whether single-tab electrodes, which are significantly less expensive and readily available in most medical centers and outpatient clinics, can provide consistent BIS measurements in BCRL patients and controls.
In an article published in the journal Lymphatic Research and Biology, they demonstrated that single-tab electrodes provide similar results to double-tab electrodes for BIS measurements when the placement of the single-tab electrode is consistent with that of the double-tab electrodes.
#Lymphedema #Understanding #Molecular #Factors