Researchers in the laboratory of Dr. Jean Cook, chair and professor of the Department of Biochemistry and Biophysics, have identified the processes of cancer cells that occur when you take an anticancer drug meant to stop the rapid growth of cells in tumors.
Cancer Cells’ Reaction to Treatments
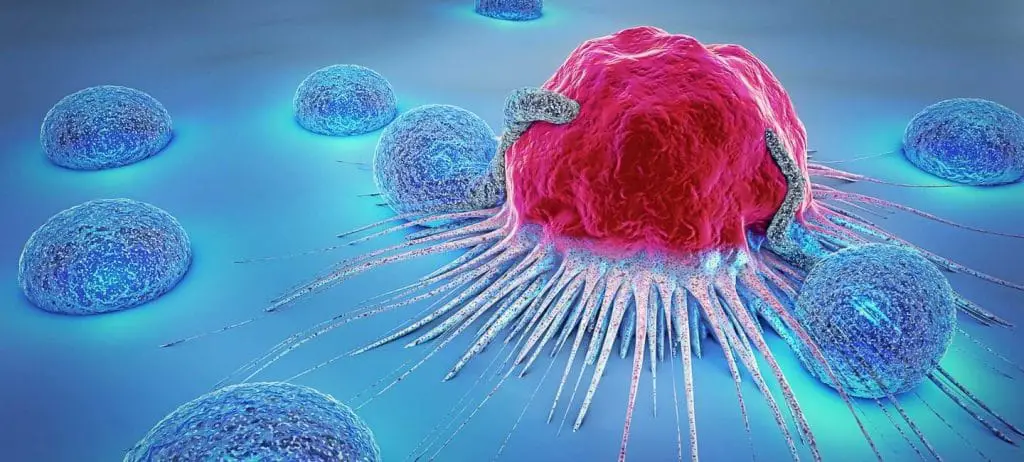
Cancer cells can hijack cell cycles to dramatically increase their numbers, a process called proliferation. Cancer drugs can stop cancer cell growth by setting off a complex chain of genetic and cellular events. But it’s often a more complex story, involving treatments that don’t work as well as hoped.
New research from Cook’s lab suggests that a particular enzyme is essential for stopping cancer cells from proliferating, particularly when patients are given cancer drugs. But the enzyme’s function is not the same in all of us. Cook’s lab has also uncovered intriguing details about how cancer cells can evade therapy designed to stop them.
Their results, published in the journal Proceedings of the National Academy of Sciences offer drug developers further food for thought in the fight against cancer.
Cells can turn genes on and off to control the expression of certain proteins. Some proteins are responsible for maintaining accurate and efficient cell division, much like musicians in an orchestra under the control of a conductor. Cells have the ability to “turn off” the controls of these regulatory proteins (for example, remove the conductor), which allows cells to divide without limit and replicate DNA for newly formed cells.
To isolate and zero in on the role that protein degradation plays in cell growth arrest, Cook and his graduate student Brandon Mouery first treated cultured human cells with palbociclib, a metastatic breast cancer drug that targets cell proliferation. Using microscopy, flow cytometry, and proteomics, the researchers found that the APC/C enzyme, which normally targets proteins for degradation to regulate the cell cycle, helps maintain the beneficial effects of palbociclib.
This finding suggests that doctors could use APC/C levels in cancerous tumors to predict how well patients might respond to palbociclib and other cancer drugs in the same class. For example, low APC/C activity could indicate that a patient might have a poor response to treatment or be at higher risk of recurrence.
Cook and Mouery also found that cancer and noncancerous cells can escape drug-induced proliferation arrest, and that escapee cells have difficulty replicating DNA on their own. One possible explanation is that they “offload” their DNA replication duties to proteins that initiate cell division late in the cell cycle. The observations suggest that cancer cells have alternative molecular pathways they can use to stimulate uncontrolled cell growth.
“Cell proliferation has been studied intensely for decades, and yet we can still be surprised,” said Cook, who is also a member of the UNC Lineberger Comprehensive Cancer Center. “In this case, we found that cancer cells can go through their cell cycle with the order of events reversed. Sometimes our textbook understanding is still pretty incomplete, so we have to keep an open mind and continually challenge paradigms.”
The new findings could lead to new interventions that can provide long-lasting proliferation-stopping effects. Combining their knowledge of this new escape route with DNA replication errors associated with cancer could open up new avenues for forcing cancer cells to grow in a “self-destructive” manner.
How Breast Cancer Cells Avoid Common Cancer Therapy
An interdisciplinary team of UNC-Chapel Hill researchers from computational medicine, genetics, biostatistics and surgery studied how cell cycle flexibility allows cancer cells to escape the effects of anticancer drugs that target cell division. UNC Lineberger members Jeremy Purvis, Ph.D., professor of genetics, and Phillip Spanheimer, MD, associate professor of surgery, led the study.
Drugs that inhibit the cancer cell cycle, such as palbociclib, have helped cure patients with the estrogen receptor-positive, human epidermal growth factor receptor-2-negative (ER+/HER2−) subtype of breast cancer. Although these drugs often improve patient outcomes, a small percentage of cancer cells survive and divide in the presence of palbociclib, a phenomenon known as fractional resistance.
Understanding the cellular mechanisms underlying fractional resistance is critical, because the precise percentage of resistant cancer cells in patient tissue is a strong predictor of clinical outcomes.
In a study published in the Proceedings of the National Academy of Sciences, a team of researchers at UNC-Chapel Hill demonstrates that fractional resistance arises from differences between cancer cells in cell cycle regulatory proteins that allow a subset of cells to escape palbociclib therapy.
The team combined multiplex single-cell imaging to identify fractionally resistant cells in both cultured and primary breast tumor samples excised from patients. The resistant cells showed premature accumulation of multiple cell cycle regulatory proteins, as well as increased sensitivity to pharmacological inhibition of cyclin-dependent kinase 2 activity, another cell division program and potential drug target.
Using computational approaches to trace the path of cancer cells through the cell cycle, the researchers demonstrate how flexibility, or plasticity, among cell cycle regulators gives rise to alternative cell cycle “pathways” that allow individual tumor cells to escape palbociclib treatment.
Understanding the drivers of cell cycle plasticity and how to eliminate resistant cell cycle pathways could lead to improved cancer therapies that target fractionally resistant cells. And improving those therapies would likely improve patient outcomes.
How to Hijack Degrading Complexes to Put Cancer Cells to Sleep
Researchers at the Universities of Newcastle and Dundee have discovered an alternative pathway through which the cancer drug palbociclib induces malignant cells to die, or senescence.
Palbociclib is a drug used to treat advanced estrogen receptor-positive breast cancer. It induces cell cycle arrest and senescence, an irreversible resting state that marks these “out of order” cells for elimination by the immune system.
In particular, the mechanistic details of how palbociclib induces cancer cells to senescence are largely unknown to date. Professor Matthias Trost from Newcastle University and colleagues from Dundee University have studied the drug’s mode of action in more detail and have discovered the proteasome, a cellular degradation mechanism vital for controlling cell proliferation, as its as yet unknown target.
Their discovery could potentially help expand palbociclib-based breast cancer treatments and identify patients who would benefit most from the drug. The research was published today in The EMBO Journal.
Palbociclib is designed to hinder tumor growth by preventing key molecules in cell cycle progression from doing their job. Specifically, it inhibits cyclin-dependent kinase 4 (CDK4) and the closely related CDK6; two factors essential for guiding cells through the DNA replication phase.
Recent observations indicate that palbociclib induces a more complete arrest than can be achieved by blocking CDK4/6. Cells treated with palbociclib irreversibly withdraw from the cell division cycle and enter a state called cellular senescence.
In this study, the researchers addressed in more detail why cells treated with palbociclib enter senescence. The researchers used a new method called thermal proteome profiling to detect cellular changes induced by palbociclib.
This technology is based on the observation of drug-induced changes in the thermal stability of cellular proteins. The method will detect proteins that bind directly to the drug or change their activity in response to the drug.
Using this approach, the researchers identified that palbociclib induced substantial changes in the proteasome, the protein complex that breaks down unnecessary or damaged proteins. More specifically, palbociclib dissociates the proteasomal component ECM29. Once freed, the proteasome degrades proteins necessary for cell cycle progression, thus pushing cells into senescence.
“Although palbociclib is known to block proliferation by inhibiting CDK4/6, induction of proteasomal activity could be an additional mechanism that ensures complete cell cycle arrest,” says Dr. Mikael Björklund, one of the study’s lead authors.
Proteasomal activity must be finely regulated to direct cells through cell division, degrading the right proteins at the right time to help the cell progress to the next stage of the division cycle. Anything that disturbs this tight regulation is likely to impede proliferation. Consequently, both activators and suppressors of proteasomal activity have been considered as treatment options for breast cancer.
The finding that palbociclib can activate proteasomal activity is important when considering potential drug combinations for the treatment of breast cancer.
“Our work suggests that proteasome inhibitors and palbociclib are not a good combination, as they act in opposite directions,” says Professor Matthias Trost of Newcastle University’s Institute of Cell and Molecular Biosciences, who co-led the study.
The researchers also found that, at least for some types of breast cancer, patients with low levels of ECM29 had longer relapse-free survival times. “ECM29 could be a biomarker to predict how responsive patients are to palbociclib. The drug would probably be more useful in patients with high levels of ECM29,” Trost says.
#Cancer #cells #divide #treatments