Scientists from the Berlin Institute of Health at Charité (BIH) and Open Targets, together with colleagues from the University of Cambridge and Addenbrooke’s Hospital in Cambridge, UK, have discovered the mechanisms that drive the regeneration of liver during chronic liver disease.
The scientists have now published their findings in the journal Nature.
The importance of liver regeneration
This regenerative process allows the liver to repair itself when it is chronically damaged, but could also cause progression to cancer.
The researchers were first able to demonstrate this by performing single-cell analyzes on many biopsies obtained from patients with steatotic liver disease associated with progressive metabolic dysfunction (MASLD). The results obtained in vivo were validated using laboratory-grown organoids.
Ludovic Vallier grows mini livers, so-called organoids, to study how liver diseases develop and how they can be treated or prevented. He is Einstein Professor for Stem Cells in Regenerative Therapies at the Berlin Institute of Health at Charité and Max-Planck-Fellow at the Max Planck Institute for Molecular Genetics. As a long-term goal, he aims to use liver organoids for cell therapies for patients with liver failure.
Steatotic steatohepatitis associated with metabolic dysfunction (MASLD) and its chronic form Steatohepatitis associated with metabolic dysfunction (MASH) is the leading cause of liver disease. It is estimated that 20-40% of the population is affected by the benign form of the disease, but currently approximately 115 million are affected by the chronic form.
Despite recent advances, the only treatment for end-stage MASH is liver transplantation, which involves heavy immunosuppressive treatment, and only a limited number of patients can benefit from this approach due to the lack of organ donors.

Therefore, Dr. Chris Gribben and Dr. Vasileios Galanakis from the Vallier team as part of an Open Targets project, in collaboration with Dr. Irina Mohorianu (Wellcome-MRC Cambridge Stem Cell Institute of the University of Cambridge) and Dr. Michael Allison (Cambridge University Hospitals NHS Foundation Trust) have turned their attention to research on this important healthcare challenge.
“We were surprised to find that relatively little is known about the mechanisms that occur during disease progression in humans. This is because studying a disease that can take decades to fully develop is very challenging. The technology needed for extensive longitudinal studies has only recently become available,” says Vallier.
The scientists collected small pieces of liver (biopsy) from patients undergoing diagnostic testing in Addenbrooke’s Hospital’s MASLD service and performed single-cell analyzes to identify the underlying mechanisms. These biopsies were collected from a large number of patients at different stages of the disease allowing for the first time to map the progression of MASLD in humans.
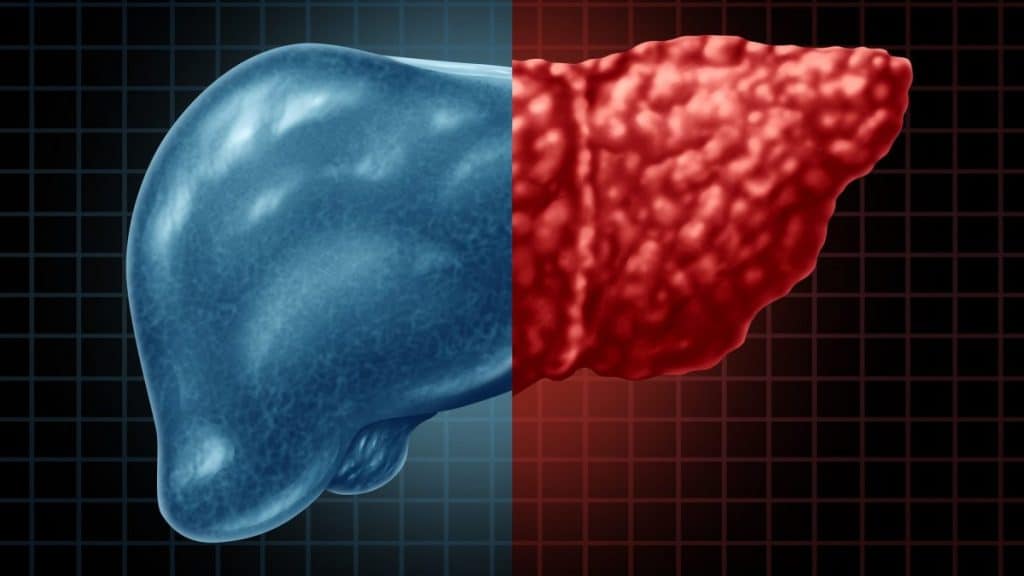
The researchers discovered an interesting mechanism: Chronic liver damage severely damages the architecture of the liver, particularly the organization of the biliary tree, which represents a network of ducts that drain the liver of toxins. This reorganization is associated with a regeneration process called transdifferentiation.
“We knew that disease progression could induce the proliferation of cholangiocytes, which are the main cell type that makes up the biliary tree. However, we did not expect this proliferation to be organized and lead to the production of such a complex network that strongly interferes with the architecture of the liver,” reports Vallier.
“Now, of course, we wanted to know whether this process was a sign that the liver was trying to repair itself or that the lesion was progressing. For this, we performed detailed analyzes on single cells and observed that cholangiocytes appear to transdifferentiate into hepatocytes, the main functional cell type of the liver, the organ then desperately tries to replace the functional cells that die during the disease,” explains Vallier .

The interesting question was to uncover the potential mechanisms behind this regenerative process: could we identify candidate factors that control regeneration? Vallier says: “We have been very fortunate to work in close collaboration with the Core Bioinformatics group led by Dr. Irina Mohorianu. Together we were able to identify a list of factors that are regulated during transdifferentiation between cholangiocytes and hepatocytes.
“These factors were then validated in tissues collected from other patients. Of particular interest, we found that insulin signaling could play an important role, thus providing an interesting avenue for future therapeutic development.”
In the next step, the scientists used cholangiocyte organoids derived from patients with progressive MASLD. These mini organs can be grown almost indefinitely in vitro while maintaining functions relevant to disease modeling.
Of particular interest is that scientists demonstrate that cholangiocyte organoids can also transdifferentiate into hepatocyte-like cells in vitro. This process could be blocked or promoted by inhibiting or increasing the insulin signaling pathway, respectively.
Furthermore, additional factors identified in patients were present in vitro, confirming the relevance of organoids for studying regenerative mechanisms in a capsule.
“We were thus able to demonstrate that molecular mechanisms that occur in humans over a prolonged period of time can be studied in vitro,” says Vallier.
The findings also suggested a more concerning aspect regarding organ regeneration.
In fact, most transdifferentiation events occur during the last phase of the disease, when the liver is extremely damaged. This regenerative process is associated with disease progression and does not appear to be directly induced by the injury.
Furthermore, end-stage liver diseases are strongly associated with liver cancer while several factors that appear to drive transdifferentiation in vivo and in vitro are also highly expressed in liver tumors. Therefore, scientists suspect that cancer may originate from regenerative processes gone awry.

In fact, chronic lesions and a diseased microenvironment could induce great stress on cells which would then become “plastic” and therefore capable of transdifferentiating. However, this acquisition of plasticity could become anomalous if it goes too far.
This study demonstrates that human organs can regenerate even after prolonged illnesses and repeated injuries. However, this process is risky and can go wrong. Controlling the acquisition of cellular plasticity is critical.
These findings cause a significant shift in our knowledge base regarding the pathophysiology of chronic liver disease. This includes the discovery of new pathways that control the balance between disease progression and tissue repair and the identification of new biomarkers for diagnostics and prognosis.
“We are obviously excited by these results,” reports Vallier, “because we believe we have found a way to develop new therapies that will not only focus on limiting disease progression but will instead aim to promote tissue repair.
“We know we need more work before this knowledge has an impact on the clinic, but this is an essential first step. We can now focus on developing new therapies, including cell-based approaches, that can ultimately help patients. And this is our goal.”
Identify the cells that help the liver heal
Scientists have discovered for the first time a type of cell responsible for repairing damaged liver tissue.
The study, which shows how these new cells migrate to the site of damage, provides new insights into how the liver heals itself. The results are published in the journal Nature.
Experts say the findings could spur the development of new therapies that exploit the liver’s unique ability to regenerate following damage.
During acute liver failure, this ability to repair and regenerate is often overwhelmed, with patients requiring an emergency liver transplant to restore liver function.
Scientists at the University of Edinburgh studied human liver tissue from patients with acute liver failure for signs of cell proliferation and regeneration following rapid loss of liver function.
They found that a significant percentage of cells retained the ability to multiply. However, substantial damaged areas were still present in the patients’ livers, suggesting that processes other than cell proliferation are critical during regeneration.
The research team profiled the genes within each liver cell in both healthy and regenerating human liver tissue to better understand the regeneration process. They did this using a cutting-edge technique called single-cell RNA sequencing.
The findings uncovered a previously undetected population of liver cells capable of healing wounds that emerge during human liver regeneration to aid recovery.
Working with scientists from the University of Glasgow at the Cancer Research UK Scotland Institute, the team used special imaging techniques in mice to observe wound-healing cells in action.
During liver regeneration, so-called leader cells appear at the edges of healthy tissue, pulling the tissue together to close the wound, similar to how skin heals after a cut.
Imaging also revealed that the healing liver cell population appears before cell proliferation begins.
Widespread infection is a major concern following acute liver failure. Bacteria from the gut can leak into the liver when the liver is damaged. This can lead to sepsis if the liver is unable to clear the infection.
The liver may prioritize wound healing before cell proliferation to restore the gut-liver barrier and prevent the spread of bacteria, experts say.
“Cutting-edge technologies have allowed us to study human liver regeneration in high definition for the first time, facilitating the identification of a cell type critical to liver repair. We hope that our findings will accelerate the discovery of much-needed new treatments for patients with liver disease,” says Professor Neil Henderson, Center for Inflammation Research, University of Edinburgh.
#Liver #regeneration #mechanisms #deciphered