Researchers at Cedars-Sinai have identified significant variations in the intestinal microbiome which are strongly associated with various body weights, from a normal body mass index, or BMI, to obesity.
The importance of the intestinal microbiome
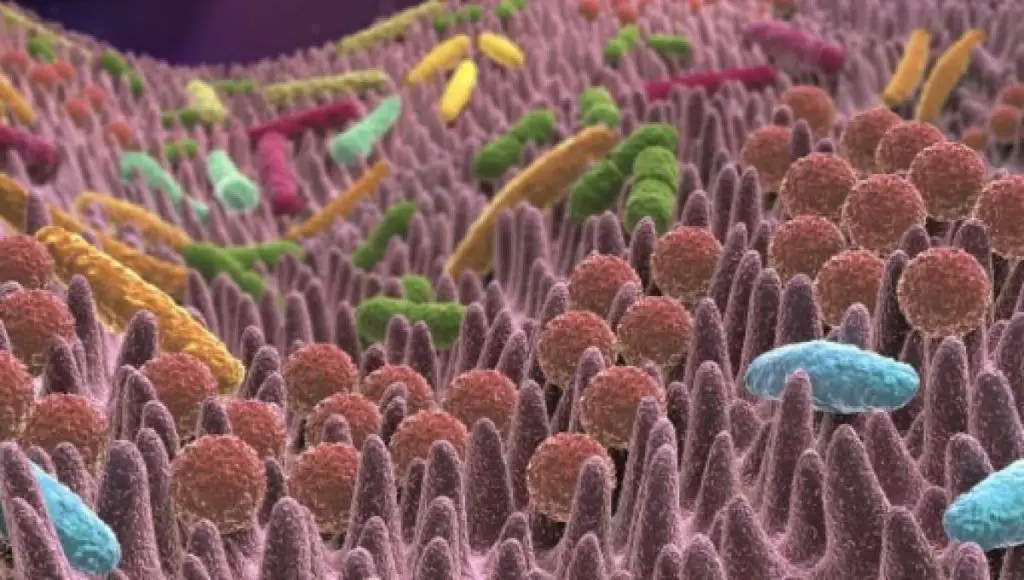
The gut microbiome includes bacteria, fungi, and viruses that populate the human gastrointestinal tract. Imbalances in these microbial populations have previously been observed in stool samples from patients with obesity-related diseases. According to the researchers, this is the first study to fully examine the small intestine microbiome in normal weight, overweight and obese subjects.
“Using specialized techniques, we took a deeper dive into the microbial universe and found that the gut microbiome of the small intestine was significantly, and specifically, altered in overweight or obese participants, compared to those of normal weight.
“Some of these changes were progressive, going from normal weight to overweight to obesity,” said endocrinologist Ruchi Mathur, MD, professor of medicine at Cedars-Sinai and corresponding author of the study published inAmerican Journal of Gastroenterology.
“Many functions related to food metabolism and nutrient absorption converge in the small intestine, as do many endocrine and immune functions that can influence weight gain.
We believe that changes in the balance of microbial populations of the small intestine's gut microbiome may have a greater impact on weight gain and the development of obesity than previously expected,” said Mathur, also director of the Training Center for outpatient diabetes teaching.
Using samples obtained from esophagogastroduodenoscopies, blood samples, and patient questionnaires, the researchers examined the gut microbiomes of 214 patients stratified by body mass index. Study participants were classified according to Centers for Disease Control and Prevention (CDC) guidelines: normal-weight subjects had a BMI between 18.5 and 24.9, overweight individuals had a BMI between between 25 and 29.9 and those classified as obese with a BMI of 30 or higher.
In all three groups, the populations of the gut microbiome of the duodenum, the first part of the small intestine where the absorption of nutrition begins, were analyzed. Shotgun metagenomic sequencing was used to obtain a comprehensive assessment of all organisms present.
“A key finding was that a bacterial population, Lactobacillus, in the duodenum showed different and highly species-specific associations in subjects classified as overweight or obese. These changes in the gut microbiome linked to weight gain may be of particular importance because many people regularly consume Lactobacillus-containing products, including dairy foods, probiotics, and some vegan dishes such as fermented tempeh,” said Gabriela Leite, Ph .D., lead author of the study and project lead scientist for the Cedars-Sinai Medically Related Science and Technology (MAST) Program.
According to the CDC, approximately 182 million adults in the United States are overweight or obese. The global number exceeds 1 billion. The causes are multifactorial and associated with serious health problems, including cardiovascular disease, metabolic syndrome and type 2 diabetes. Genetics, epigenetics, gut hormones and the gut microbiome are involved in the pathophysiology of obesity, which can also be influenced by socioeconomic and psychosocial factors.

Researchers believe that understanding the influences and activity of the gut microbiome that populates our small intestine microbiome may offer an important path to improving the health and lives of millions of people.
“Identifying changes in the populations and activity of small intestinal microbial species associated with overweight or obesity is part of a key initiative to develop new therapeutic targets and personalize medicine,” said the gastroenterologist and study co-author Mark Pimentel, MD, executive director of Cedars-Sinai's MAST program.
“Further research will be needed to identify cause-and-effect relationships between the changes we observed, but the goal is to develop treatments and interventions that help people reduce their risk of obesity-related diseases and improve their overall health.” , Pimentel said.
Age and aging have critical effects on the gut microbiome
Cedars-Sinai researchers have found that aging produces significant changes in the human gut microbiome distinct from those caused by medications or disease burden. The results were published in the journal Cell Reports.
“By highlighting the microbial changes that occur in the small intestine with age, drug use and disease, we hope to identify unique components of the microbial community to target for therapies and interventions that could promote healthy aging,” he said Ruchi Mathur, MD, the study's principal investigator.
According to Mathur, research exploring the gut microbiome and its impact on health has predominantly relied on fecal samples, which do not represent the entire gut. In their study, researchers from Cedars-Sinai's Medically Associated Science and Technology (MAST) program analyzed samples of the small intestine — which is more than 20 feet long and has the surface area of a tennis court — to examine the microbiome and its relationship with aging.
“This study is the first of its kind to examine the microbial composition of the small intestine of subjects aged 18 to 80 years. We now know that some microbial populations are more affected by drugs, while others are more affected by certain diseases. We have identified specific microbes that appear to be influenced only by the person's chronological age,” said Mathur, an endocrinologist and director of the Diabetes Outpatient Treatment & Education Center.

The 21st century has been called the “age of the gut microbiome” as scientists pay close attention to the role that trillions of gut bacteria, fungi, and viruses can play in human health and disease. The microbiome is the name given to the genes that live in these cells. Studies have suggested that disturbances in the constellations of the microbial universe can lead to critical diseases, including gastroenterological diseases, diabetes, obesity and some neurological disorders.
While researchers know that microbial diversity in stool decreases with age, Cedars-Sinai researchers have identified bacteria in the small intestine that they call “disturbers” that increase and could be bothersome.
“Coliforms are normal residents of the intestine. We found that when these rod-shaped microbes become too abundant in the small intestine, as they do as we age, they exert a negative influence on the rest of the microbial population. They are like weeds in a garden,” said study co-author Gabriela Leite, Ph.D.
The researchers also found that as people age, the bacteria in the small intestine change from microbes that prefer oxygen to those that can survive on less oxygen, something they hope to understand as research into the gut microbiome continues.
“Our goal is to identify and detect small intestinal microbial patterns of human health and disease. Given the important role the small intestine plays in nutrient absorption, changes in the microbiome in this location of the gut could have a greater impact on human health.” , and deserves further study,” said Mark Pimentel, MD, director of the MAST program and co-author of the study.
This research is part of Cedars-Sinai's ongoing REIMAGINE study: Revealing the Whole Intestinal Microbiota and its Associations with the Genetic, Immunologic, and Neuroendocrine Ecosystem.
Antibiotics affect male and female gut microbiomes differently
In an additional study, Cedars-Sinai researchers found that antibiotics have sex-specific effects on the composition of the gut microbiome of male and female laboratory rats.
The findings, published in the journal Frontiers in Microbiology, could have implications for the drugs' use in humans to treat or prevent bacterial infections.
“We found that giving rats a multidrug antibiotic cocktail produced significant, sex-specific changes in both the feces, or large intestine, and the small intestine. For example, a greater loss of microbial diversity in both the stool and the small intestine.” was observed in male rodents compared to female,” said Ruchi Mathur, MD, the study's principal investigator.

“Changes in the diversity of the gut microbiome could have a negative impact. Previous studies on gut health have shown that overall microbial diversity promotes vitality and resilience, often contributing to a healthier gut,” said Mathur, an endocrinologist.
In the controlled study, researchers from the Cedars-Sinai Medically Associated Science and Technology (MAST) program compared the composition of the gut microbes of male and female rats before, during, and after treatment with broad-spectrum antibiotics, including vancomycin, ampicillin, metronidazole and neomycin.
“We followed the rats for a period after stopping the antibiotics and found that many of the sex-specific changes observed during treatment remained. The constellation of microbes in the gut did not return to their original pre-antibiotic composition in either sex. throughout the duration of the study,” said research associate Gonzalo Parodi, first author of the article.
Some studies have identified sex-specific effects of antibiotics on the large intestine (stool) microbiome in mice. But the Cedars-Sinai researchers point out that this is the first study to also examine changes in the small intestine microbiome induced by antibiotics and to also use male and female rats that had no significant differences in microbiome composition before treatment.

“It is difficult to pinpoint the impact of drugs if the gut microbiomes of laboratory animals are different from the start. We used rats with similar gut profiles straight out of the gate. This allowed us to identify changes in the microbiomes of male and female rats that could be specifically attributed to the impact of antibiotics during and after drug exposure,” said Mark Pimentel, MD, director of the MAST program and co-author of the study .
Further studies using different combinations of antibiotics and exposure times are needed. The investigators say that if these findings hold true for humans, the research could have implications for how antibiotics are prescribed.
“Sex is a biological variable and, like any variable, must be taken into account in medical and basic research. Currently, when we administer medications to patients, we consider factors such as kidney function and weight. Depending on the results of further research, particularly in humans, patients' gender may one day be an important consideration when prescribing antibiotics,” Mathur said.
#Intestinal #microbiome #variations #related #body #weight
