The liver it is the largest internal organ of the human body. It is necessary for hundreds of bodily processes, including the breakdown of toxins such as alcohol. Since it is the first organ to “see” the alcohol that has been drunk, it is not surprising that it is the most susceptible to the effects of alcohol. However, other organs, including the brain and heart, can also be damaged by long-term excessive alcohol consumption.
Liver damage from excessive alcohol consumption
According to Greek mythology, Zeus punished Prometheus for giving fire to humans. He chained Prometheus and set an eagle to feast on his liver. Every night the organ grew again and every day the eagle returned to feast on him. In fact, can it really grow back?
Alcohol initially makes the liver fatty. This fat causes liver inflammation. In response, it tries to heal itself, producing scar tissue. If this continues unchecked, the entire organ can become a network of scars with little islands of “good” liver in between: cirrhosis.
In the advanced stages of cirrhosis, when the organ is not functioning well, people may become yellow (jaundice), swell with fluid, and become drowsy and confused. This is serious and can be fatal.
Most people who regularly drink more than the recommended limit of 14 units of alcohol per week (about six pints of regular-strength beer [4% ABV] or about six medium glasses of wine [175 ml] [14% ABV]) will have hepatic body fat. Excessive and prolonged alcohol consumption increases the risk of developing scars and cirrhosis.
Fortunately there is good news. In people with fatty liver, after just two to three weeks of giving up alcohol, the organ can heal and look and function like new.
In people with liver inflammation or mild scarring, even within seven days of giving up alcohol, notable reductions in liver fat, inflammation and scarring are seen. Stopping alcohol use for several months allows the liver to heal and return to normal.
In heavy drinkers with more severe scarring or liver failure, giving up alcohol for several years reduces the chance of worsening liver failure and death. However, people who drink heavily can be physically dependent on alcohol, and suddenly stopping drinking can cause alcohol withdrawal.

In its mild form it causes tremors and sweating. But if severe, it can cause hallucinations, seizures and even death. Going “cold” is never recommended for heavy drinkers, who should seek medical advice on how to safely give up alcohol.
Quitting drinking also has positive effects on sleep, brain function and blood pressure.
Avoiding alcohol for long periods also reduces the risk of several types of cancer (including liver, pancreas, and colon) and the risk of heart disease and stroke.
However, alcohol is not the only cause of health problems. Giving up has many health benefits, but it is not a panacea. It should be seen as part of a healthy lifestyle, including a balanced diet and regular exercise.
So, to answer the question posed by the Prometheus myth, the liver has an extraordinary power to repair itself after it has been damaged. But it cannot grow back as good as new if it was already severely scarred.
If you stop drinking and just have fatty liver, it can quickly return to normal. If you initially had liver scarring (cirrhosis), stopping drinking alcohol will allow for healing and improved function, but will not undo all the damage that has already been done.
If you want to take care of your liver, drink in moderation and spend two or three days without alcohol each week. This way, you won't have to rely on magical self-healing power to stay healthy.
How much drinking too much damages the liver
Between March 2020 and January 2021, the number of U.S. patients with alcohol-associated liver disease who received a new liver or were on the waiting list for a transplant was 50% higher than pre-pandemic projections, the researchers say. researchers.
Alcohol-associated liver disease is now the leading reason for liver transplants in the United States.
“The general rule is more than two drinks a day for men, more than one drink a day for women puts you at risk,” said Dr. Karen Krok. She is a gastroenterologist and hepatologist at Penn State Health Milton S. Hershey Medical Center in Hershey, Pennsylvania.
Alcohol creates fatty deposits in the liver that eventually cause scarring (cirrhosis), which is a form of liver disease associated with alcohol.
Another is alcohol-associated hepatitis, which occurs when the liver becomes inflamed by drinking too much alcohol in a short time.
In the early stages of alcohol-associated liver disease, a person may have elevated liver enzyme levels but may otherwise show no symptoms. Eventually, elevated liver enzymes can lead to jaundice, the yellowing of a person's eyes or skin.

Other symptoms include fluid accumulation in the belly; dilated blood vessels in the esophagus that may bleed; and mental confusion caused by the accumulation of toxins in the blood that would normally be removed by the liver.
If a person with alcohol-associated liver damage stops drinking, their symptoms can be treated with medications, experts noted. But some patients require a liver transplant.
About 7,000 liver transplants are performed each year in the United States, and the average survival rate is 91% after one year and 75% after five years, according to a press release from Penn State Health.
In addition to making sure a patient is physically capable of undergoing a liver transplant, we must “make sure the patient follows medical recommendations and protects that organ,” said Dr. Juan Arenas, chief of the Division of Transplant Surgery at Hershey Medical Center.
“Social support is very important to help patients get through difficult times, come to appointments and stay away from the substance that led to liver disease,” he added.
Alcohol consumption in patients with chronic liver disease
A review article published in the New England Journal of Medicine discusses the effects of alcohol consumption on various forms of liver disease, as well as the evaluation and treatment of alcohol consumption in patients with chronic liver disease.
Liver-related mortality is increasing worldwide, largely due to increased alcohol consumption. This review is highly timely, as recent epidemiological studies have shown that alcohol consumption that does not reach the risk range is associated with increased morbidity and mortality.

Below is a summary of the review article:
Alcohol consumption is common among patients with liver disease and is associated with poor outcomes. Additionally, advanced liver disease can complicate the pharmacologic treatment of alcohol use disorder and alcohol withdrawal syndrome. In fact, medications approved for alcohol use disorder are prescribed to a minority of patients, but could be used by patients with chronic liver disease.
Given that there is no safe threshold for alcohol consumption and, if there is, it is probably very low, abstinence should be encouraged in patients with chronic liver disease. Additionally, liver transplant might be considered for patients who abstain from alcohol and have progressive liver failure.
The authors conclude that the treatment of alcohol use disorders should be expanded into daily clinical practice to include patients with advanced liver disease.
Liver cancer caused by alcohol consumption may have a worse prognosis than other forms
A further study indicates that patients with liver cancer alcohol-related liver cancer often do not live as long as patients with liver cancer not associated with alcohol consumption, mainly due to diagnoses at later stages. Initially published online in Cancer, a peer-reviewed journal of the American Cancer Society, the findings indicate that efforts should be made to improve both screening for early signs of liver cancer and management of alcohol abuse.
Liver cancer is the second leading cause of cancer-related death worldwide, with hepatitis B and C infections being the leading causes. Alcohol abuse and non-alcoholic fatty liver disease are other dominant risk factors.
Due to improvements in the treatment of hepatitis infections and increased alcohol consumption in some regions, alcohol is likely to become a leading cause of liver cancer in the near future.
In fact, alcohol is already the leading cause of liver cancer in France and is involved in 25-30% of diagnoses in the United States. The true figure in the United States is likely higher because alcohol consumption is often underreported when another risk factor is present.
To compare aspects of alcohol-related and non-alcohol-related liver cancer, Charlotte Costentin, MD, of Hôpital Henri-Mondor in France, and her colleagues examined 894 patients with newly diagnosed liver cancer who were followed for 5 years; 582 patients (65%) had a history of chronic alcohol abuse and 312 (35%) did not. The researchers also recorded whether patients with alcohol-related liver cancer were abstinent or not at the time of their cancer diagnosis.
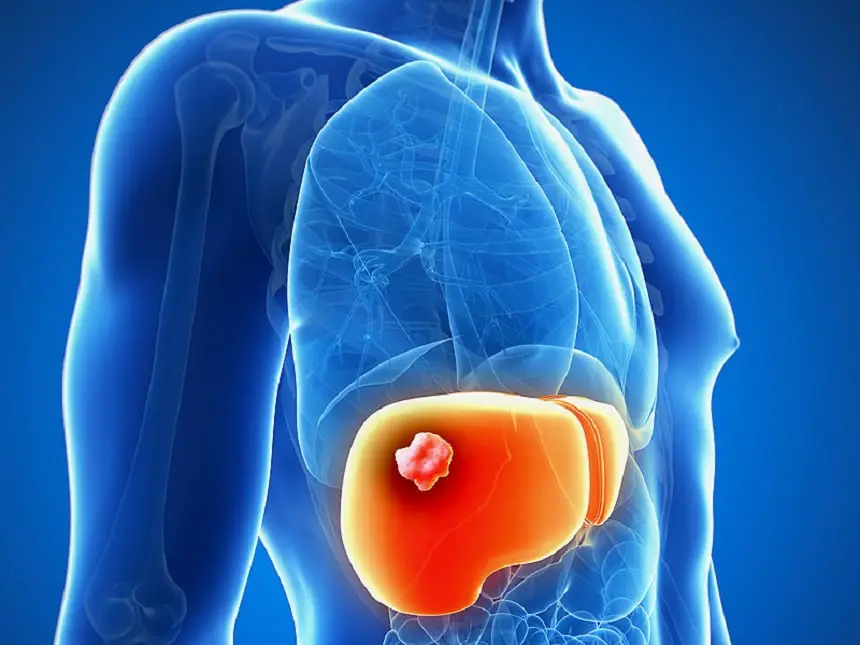
At the time of the investigators' final analyses, a total of 601 patients had died. Alcohol-related liver cancers were more likely to be widespread and were detected in patients with worse liver function. Median overall survival was 9.7 months versus 5.7 months in the non-alcohol-related and alcohol-related groups, respectively. When researchers looked at each cancer stage individually, however, survival was similar in patients with non-alcohol-related and alcohol-related cancer.
The findings suggest that patients with alcohol-related liver cancer have reduced overall survival primarily due to worsening liver function and tumor characteristics at the time of diagnosis.
The analysis also looked at whether patients participated in follow-up programs for cirrhosis before they were diagnosed with cancer. (Most people who develop liver cancer show signs of scarring, or cirrhosis, in the liver, and international guidelines recommend ultrasound every six months to detect early liver cancer in patients with cirrhosis.) Patients whose liver cancer was detected during follow-up for cirrhosis The program had improved survival compared with patients whose cancer was diagnosed incidentally.

This was especially pronounced in patients with non-alcohol-related liver disease or in those with alcohol-related liver disease who no longer drink alcohol compared to non-abstinent patients. Additionally, non-abstinent alcoholic patients had the lowest survival in the study, even when limiting the analysis to patients involved in cirrhosis follow-up programs.
“To improve the prognosis of liver cancer in the alcoholic population, efforts should be made to implement effective screening programs for both cirrhosis and liver cancer, and to improve access to alcoholism treatment services,” he said. stated Dr. Costentin.
“Lower tumor burden and better liver function at the time of diagnosis should result in higher rates of patients with alcohol-related liver cancer amenable to curative treatment such as tumor resection or liver ablation and transplantation.”
#Here39s #liver #stop #drinking