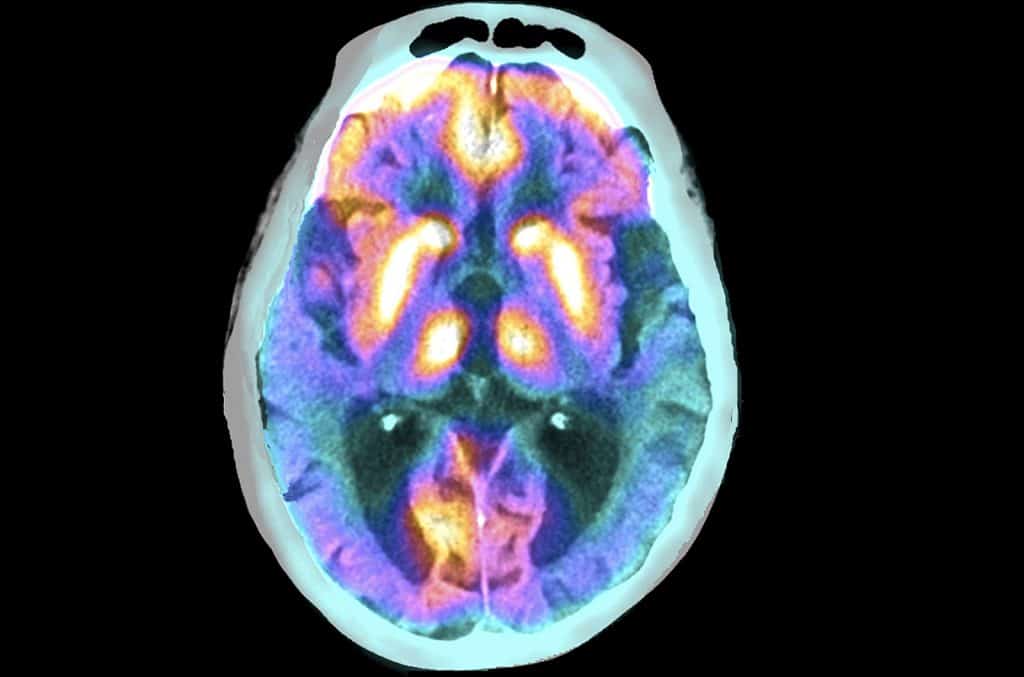
Researchers at the Icahn School of Medicine at Mount Sinai have made a significant breakthrough in research on Alzheimer’s disease identifying a new way to slow or even stop the progression of the disease.
The study, which focuses on the role of reactive astrocytes and the plesin-B1 protein in the pathophysiology of AD, provides crucial insights into brain cell communication and opens the door to innovative treatment strategies. It was published in Nature Neuroscience on May 27. identifying a new way to slow or even stop the progression of the disease.
The research was published on Nature Neuroscience.
A significant step forward in research into Alzheimer’s disease
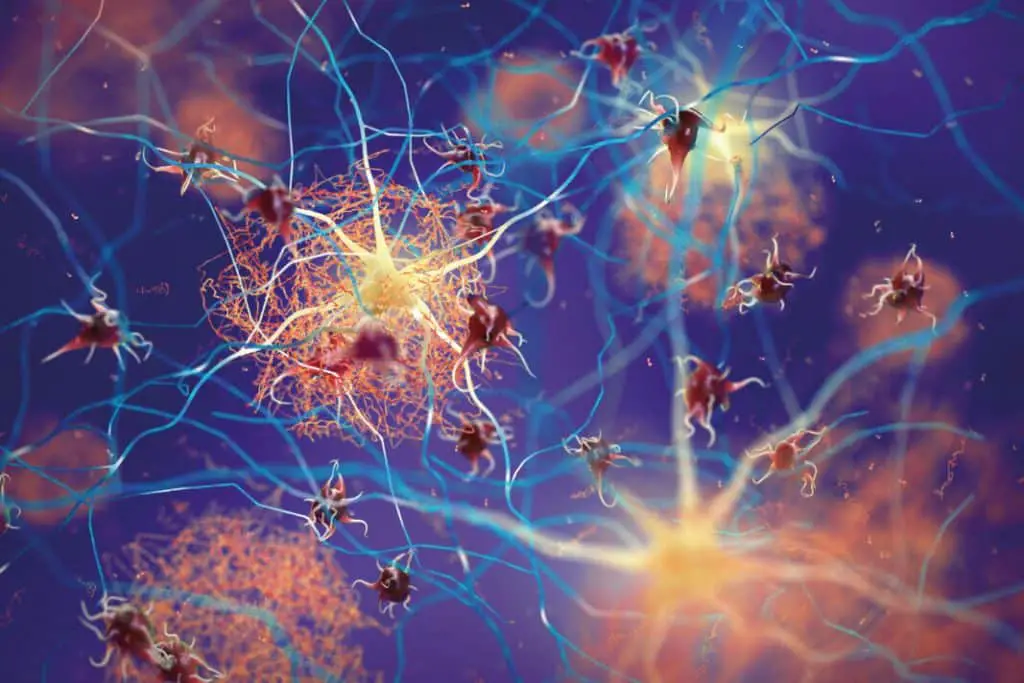
This work focuses on manipulating the protein plexin-B1 to improve the brain’s ability to clear amyloid plaques, a hallmark of AD disease.
Reactive astrocytes, a type of brain cell that activates in response to injury or disease, have been found to play a crucial role in this process. They help control the space around amyloid plaques, influencing how other brain cells can access and eliminate these harmful deposits.
“Our findings offer a promising path for developing new treatments by improving how cells interact with these harmful plaques,” said Roland Friedel, Ph.D., associate professor of Neuroscience and Neurosurgery at Icahn Mount Sinai and senior author of the study.
The research was guided by the analysis of complex data comparing healthy individuals with those suffering from AD, with the aim of understanding the molecular and cellular basis of the disease.
Hongyan Zou, Ph.D., Professor of Neurosurgery and Neuroscience, at Icahn Mount Sinai and one of the study’s lead authors, highlighted the broader implications of their findings: “Our study opens new avenues for AD research , highlighting the importance of cell interactions in the development of treatments for neurodegenerative diseases.”
One of the study’s most significant findings is the validation of multiscale genetic network models of AD disease.
“This study not only confirms one of the most important predictions of our genetic network models, but also significantly advances our understanding of AD. It lays a solid foundation for the development of new therapies targeting such highly predictive network models,” said Bin Zhang, Ph.D., Willard TC Johnson Research Professor of Neurogenetics at Icahn Mount Sinai and one of the study’s lead authors.
By demonstrating the critical role of plesin B1 in Alzheimer’s disease, the research highlights the potential of targeted therapies to halt disease progression.
The research team emphasizes that although their findings mark significant progress in the fight against Alzheimer’s, further research is needed to translate these findings into treatments for human patients.
“Our ultimate goal is to develop treatments that can prevent or slow the progression of Alzheimer’s,” added Dr. Zhang, outlining the team’s commitment to further exploring the therapeutic potential of plesin-B1.
Key role of DNA methylation in Alzheimer’s disease
Mount Sinai researchers have published a study in Alzheimer’s & Dementia: The Journal of the Alzheimer’s Association that sheds new light on the role of DNA methylation in Alzheimer’s disease (AD).
The study found that DNA methylation has a profound impact on gene and protein co-expression networks associated with AD and could lead to the discovery of new neuropathological processes and molecular mechanisms for the development of new treatments for the disease
The study was conducted using a novel analytical approach to quantify the impact of DNA methylation on gene and protein expression and a large cohort of postmortem, mild cognitive impairment (MCI), and AD control brains from Mount Sinai Brain. Bank.
The researchers profiled genome-wide methylomic changes in the parahippocampal gyrus, a brain region involved in a variety of functions including memory processing, and studied the influence of these changes on mRNA and protein co-expression networks. .
They discovered 270 distinct differentially methylated regions (DMRs) in AD compared to normal controls and validated their key findings using an independent cohort (Religious Orders Study and Memory Assessment Project, ROSMAP).
“Our study represents the first comprehensive effort to integrate high-throughput multi-omics profiling into Alzheimer’s disease,” said senior author, Bin Zhang, Ph.D., Willard TC Johnson Research Professor of Neurogenetics and Director from the Mount Sinai Center for Transformative Disease Modeling.
“It provides a framework for future data integration at the multiscale network level and could lead to the discovery of new targets for drug discovery against Alzheimer’s disease.”
The results of this study offer a new approach to investigate the relationship between DNA methylation and gene/protein expression and highlight the importance of epigenetic mechanisms in human diseases such as AD.
The researchers plan to extend their methods to study methylomic variation and impacts on multiscale networks at the single-cell level, which could provide new insights into the DNA methylation profiles of individual cell types.
Diabetes medications can reduce the severity of Alzheimer’s disease
People with Alzheimer’s disease who were treated with diabetes drugs showed considerably fewer disease markers – including abnormal microvasculature and dysregulated gene expressions – in the brain than Alzheimer’s disease patients without diabetes treatment, report researchers at Mount Sinai.
The results of the study will be published in PLOS One online.
This is the first study to examine what happens in the pathways of both brain tissue and endothelial cells – the cells that line blood vessels – in the brains of Alzheimer’s patients treated with diabetes drugs.
The study’s findings will inform future Alzheimer’s disease studies and potential new therapies targeting specific cells, as they suggest that targeting the brain’s capillary system could have beneficial effects in Alzheimer’s patients.
Many older adults with diabetes have brain changes that are hallmarks of Alzheimer’s. Despite this link, two previous Mount Sinai studies of brain tissue found that the brains of people with Alzheimer’s disease and diabetes had fewer Alzheimer’s lesions than the brains of people with Alzheimer’s disease without diabetes. The findings suggested that antidiabetic drugs had a protective effect on the brains of Alzheimer’s disease patients.
To determine what happens at the molecular level, this Mount Sinai research team developed a method to separate brain capillaries from the brain tissue of 34 people with Alzheimer’s and type 2 diabetes who had been treated with anti-diabetes drugs and compare them with tissue from 30 people. brains from people with Alzheimer’s without diabetes and 19 brains from people without Alzheimer’s or diabetes.

Because most people with diabetes are treated with insulin or oral medications, the scientists were unable to compare their findings with brain tissue from people with Alzheimer’s disease and diabetes who had not been treated with antidiabetic drugs.
Then, they examined vessels and brain tissue separately to measure Alzheimer’s disease-associated changes in RNA molecular markers for brain capillary cells and insulin signaling.
Levels of about half of these markers were reduced in vessels and brain tissue in the Alzheimer’s and diabetes group. The vast majority of RNA changes seen in Alzheimer’s disease were absent in Alzheimer’s patients who had been treated with antidiabetic drugs.
“The results of this study are important because they provide us with new insights into the treatment of Alzheimer’s disease,” said the study’s senior author, Vahram Haroutunian, Ph.D., Professor of Psychiatry and Neuroscience at the Icahn School of Medicine of Mount Sinai.
“Most modern Alzheimer’s treatments target amyloid plaques and have failed to effectively treat the disease,” Dr. Haroutunian said.
“Insulin and diabetes medications such as metformin are FDA-approved and safely administered to millions of people and appear to have a beneficial effect on people with Alzheimer’s. This opens up opportunities to conduct research studies on people who use similar drugs or on drugs that have similar effects on Alzheimer’s. the brain’s biological pathways and cell types identified in this study.”
#Alzheimers #stop #progression #disease
