New research suggests that the vaccine HPV It prevents cancer in men, as well as women, but fewer boys than girls are vaccinated in the United States.
The results of the study and a second were published Thursday byAmerican Society of Clinical Oncology and will be discussed in June 2024 at its annual meeting in Chicago. The second study shows that vaccination rates are increasing, but males lag behind females in HPV vaccination.
The importance of the HPV vaccine
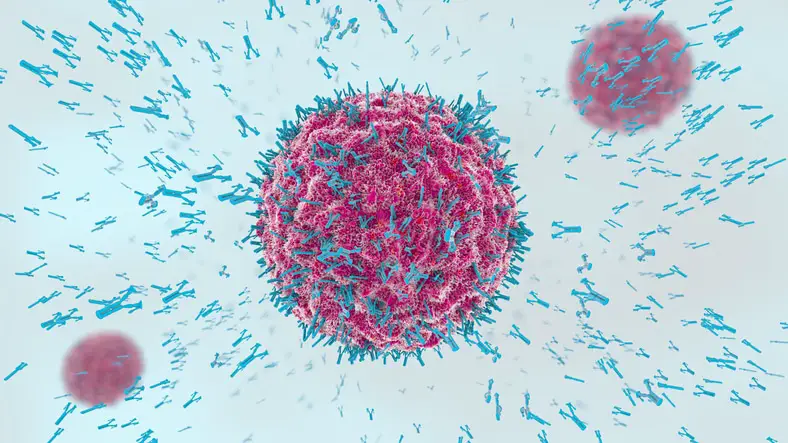
The HPV vaccine was developed to prevent cervical cancer in women, and experts credit it, along with screening, with reducing cervical cancer rates. Evidence that vaccinations prevent HPV-related cancers in men has emerged more slowly, but new research suggests that vaccinated men have fewer mouth and throat cancers than those who did not receive vaccinations. These cancers are more than twice as common in men than in women.
For the study, researchers compared 3.4 million people of similar age – half vaccinated and half unvaccinated – across a large health data set.
As expected, vaccinated women had a lower risk of developing cervical cancer within at least five years of vaccination. There were advantages for men too. Vaccinated men had a lower risk of developing any HPV-related cancers, such as cancers of the anus, penis, mouth and throat.
These cancers take years to develop, so the numbers were low: There were 57 HPV-related cancers among unvaccinated men — mostly head and neck cancers — compared with 26 among men who had received the HPV vaccine .
“We think the maximum benefit from the vaccine will actually be achieved over the next two to three decades,” said study co-author Dr. Joseph Curry, a head and neck surgeon at the Sidney Kimmel Cancer Center in Philadelphia. “What we are showing here is a first wave of effects.”
HPV, or human papillomavirus, is very common and is transmitted through sex. Most HPV infections cause no symptoms and clear up without treatment. Others develop into cancer, about 37,000 cases per year, according to the Centers for Disease Control and Prevention.
In the United States, the HPV vaccine has been recommended since 2006 for girls aged 11 or 12 and since 2011 for boys of the same age. Catch-up shots are recommended for anyone who has not been vaccinated up to age 26.
In the second study, researchers examined self- and parent-reported HPV vaccination rates in preteens and young adults in a large government survey. From 2011 to 2020, vaccination rates increased from 38% to 49% among females and from 8% to 36% among males.
“HPV vaccine uptake among young males has increased more than fourfold over the past decade, although vaccination rates among young males are still lower than among females,” said study co-author Dr. Danh Nguyen at the University of Texas Southwestern Medical Center at Dallas.
Parents of boys, as well as girls, should know that HPV vaccines reduce the risk of cancer, said Jasmin Tiro of the University of Chicago Medicine Comprehensive Cancer Center, who was not involved in the research. And young people who have not been vaccinated can still get vaccinated.
“It’s really important that adolescents are exposed to the vaccine before they are exposed to the virus,” she said.
the link between HPV and throat cancer
There are more than 100 strains of HPV. Some types of viruses can cause cancer. HPV 16 has been linked to increased cases of oropharyngeal cancer, commonly known as throat cancer. It is the most common HPV-associated cancer in men, and the infection rate continues to increase. These tumors are treatable, but prevention is always better, starting with the HPV vaccine.
“It is a vaccine recommended for all boys and girls, at the age of 11 and 12. This is when it is on the routine recommendation list for vaccines, even though you can actually give it as early as 9 years old,” says Dr. Price. The vaccine is available for people up to age 45.
“It’s much better to get a safe vaccine that has no side effects or long-term complications than to have to go through surgery, radiation and chemotherapy,” says Dr. Price.
The Centers for Disease Control and Prevention has more information on vaccine dosing and schedule for children and adults. Along with vaccination, you can reduce risks by avoiding tobacco and limiting alcohol consumption. HPV infection is often asymptomatic and can lead to cancer of the cervix, vagina, vulva, penis, anus, and throat .
92% of cancers caused by HPV could be prevented with the vaccine
An estimated 92% of cancers caused by HPV could be prevented through vaccination, the US Centers for Disease Control and Prevention (CDC) said on Thursday, adding that increasing vaccination coverage is a key priority.
According to a study published by the CDC, the human papillomavirus was responsible for an estimated annual average of 34,800 cancer cases between 2012 and 2016, meaning that more than 32,100 cases could have been prevented each year.
The virus can lead to cancers in both men and women, including cancers of the cervix, vulva, vagina, penis, anus, and oropharynx (the back of the throat, including the base of the tongue and tonsils ).
“An HPV-free cancer-free future is within reach, but urgent action is needed to improve vaccination coverage rates,” said Brett Giroir, Assistant Secretary of Health.
“Increasing HPV vaccination coverage to 80% has been and will continue to be a priority initiative for HHS, and we will continue to work with our government and private sector partners to make it a reality.”
The CDC recommends that all preteens receive the HPV vaccine when they are 11 or 12 years old to protect them before they are exposed.
But the new data showed little progress in increasing vaccination rates among young people aged 13 to 17.
Overall, only 51% of teens received all recommended doses, an increase of two percentage points from 2017, with vaccination rates higher among teens whose parents received a recommendation from their doctor.
The report adds that while the vaccine is not normally recommended for people over the age of 26, some adults aged 27 to 45 who have not previously been vaccinated may benefit from it if they are at risk and should speak to their doctor for advice.
HPV vaccination is also key to preventing cervical cancer, the report adds, recommending a Pap test every three years along with an HPV test in women ages 21 to 29.
“HPV testing can provide additional information when Pap test results are unclear for women aged 21 years and older,” the report states.
HPV vaccination rates increasing among adolescents
Human papillomavirus (HPV) vaccination coverage increased 5.1 percentage points from 2016 to 2017, and there was also an increase in the number of adolescents up to date with HPV vaccinations, according to research published in the 24th issue. August of the U.S. Centers for Disease Control and Prevention’s Morbidity and Mortality Weekly Report.
Tanja Y. Walker, MPH, of the CDC in Atlanta, and colleagues analyzed data from the 2017 National Immunization Survey-Teen for 20,949 adolescents ages 13 to 17 to estimate adolescent vaccination coverage.
Norovirus, the highly contagious gastrointestinal disease, is best known for rapidly spreading in elderly homes, schools and other densely populated spaces, numbering approximately 200,000 people annually, the majority of which are in the developing world. There is no treatment or medicine to prevent illness, and scientists have little understanding of how the infection begins.
ESPAÑA EUROPE MADRID HEALTH
CDC
The researchers found that coverage increased for one or more doses of HPV vaccine (from 60.4 to 65.5%), one or more doses of meningococcal conjugate vaccine (MenACWY; from 82.2 to 85.1%). ) and two or more doses of MenACWY (39.1 to 44.3%). ) from 2016 to 2017.
Vaccination coverage against tetanus, reduced diphtheria toxoids and acellular pertussis (Tdap) remained stable at 88.7%. Compared to 43.4% in 2016, 48.6% of youth were up to date with the HPV vaccine series in 2017. There has also been an increase in on-time vaccinations.
Although HPV vaccination initiation remains lower than coverage with MenACWY and Tdap, HPV vaccination coverage has increased by an average of 5.1 percentage points per year since 2013, indicating that ongoing efforts to Targeting unvaccinated adolescents and eliminating missed vaccination opportunities could lead to levels of HPV vaccination coverage comparable to those of other vaccines routinely recommended for adolescents,” the authors write.
#HPV #vaccines #prevent #cancer #men #women
